Final Thoughts on ACLS Tachycardia Algorithm
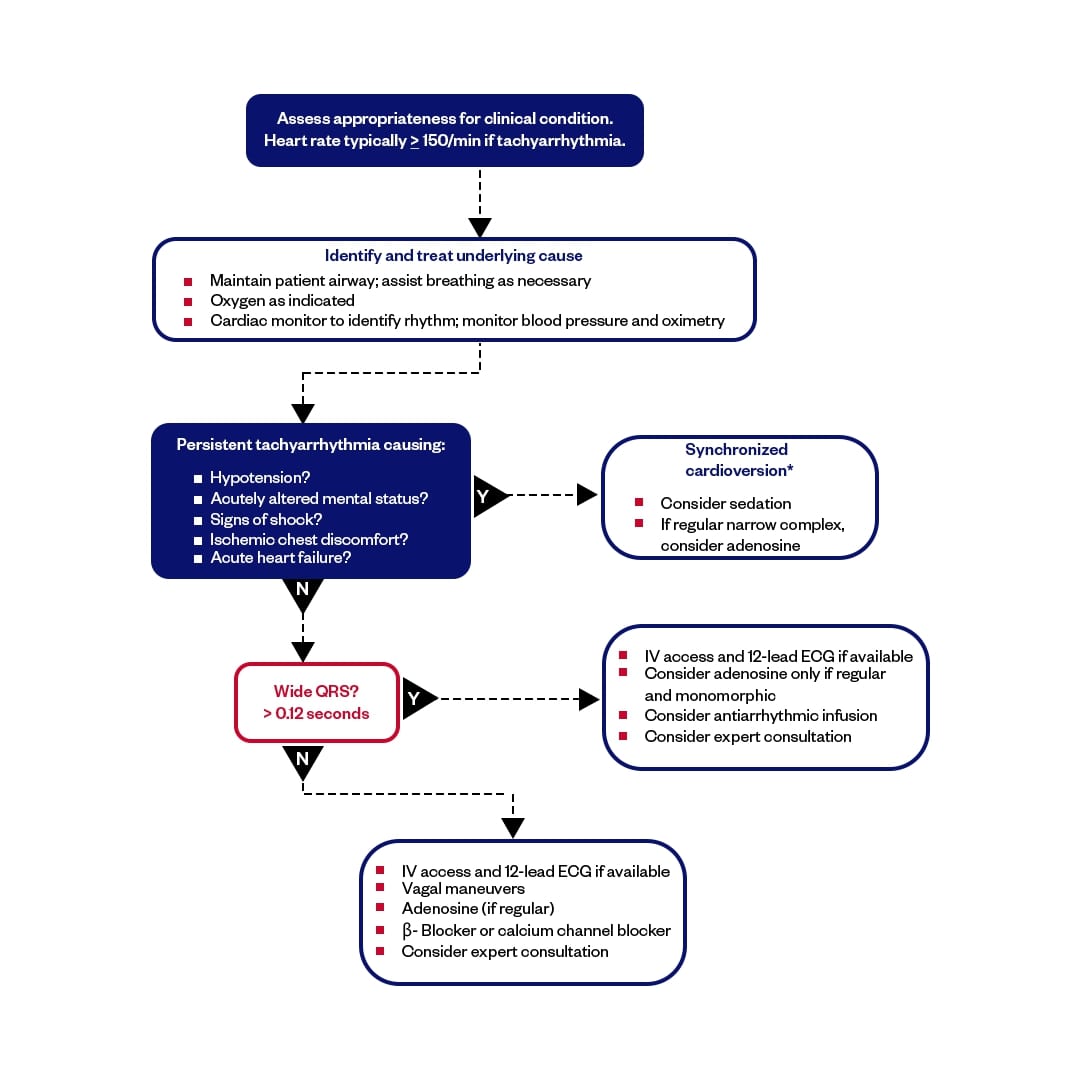
The ACLS adult tachycardia algorithm offers a clear, step-by-step approach to assess and manage patients experiencing rapid heart rhythms. It is crucial to understand when to provide basic support, how to evaluate patient stability, and when to apply medications or electrical therapy to improve outcomes during tachycardia emergencies. Mastery of this algorithm ensures timely and effective treatment that can save lives.
The ACLS Tachycardia Algorithm is an essential tool for healthcare professionals aiming to build confidence and hands-on skills in managing tachycardia emergencies. By joining CPRVAM, you gain access to expert-led courses offering practical training and comprehensive knowledge, helping you become proficient in advanced cardiac life support. Start your learning journey today and be prepared to respond swiftly and effectively when every second counts.