Rescuer Pediatric
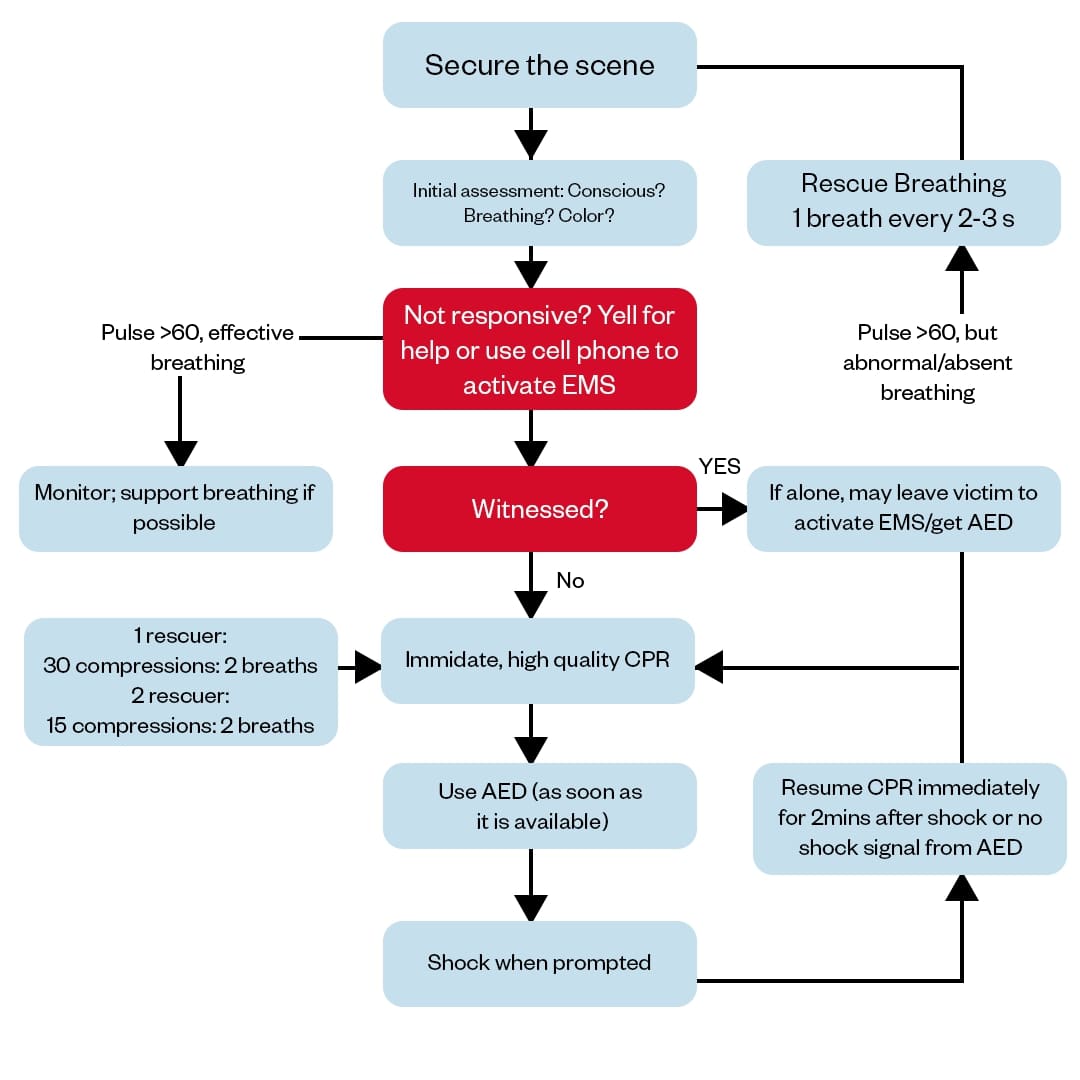
- Assess the scene.
- Check responsiveness.
- Activate emergency response (call for help and, if available, retrieve an AED).
- Check pulse for no more than 10 seconds.
- If there is no pulse, start CPR with chest compressions at a rate of 100-120 per minute.
- After 30 compressions, give 2 rescue breaths.
- Continue the cycle of 30 compressions followed by 2 breaths until help arrives or the child starts breathing on their own.