Pediatric emergencies are high-pressure situations where every second counts, from a newborn struggling to breathe to a school-aged child experiencing severe asthma or a teen collapsing from cardiac arrest. Pediatric Advanced Life Support (PALS) Megacodes prepare healthcare providers to act quickly and effectively. These hands-on simulations recreate real-life scenarios, testing skills in rapid assessment, interventions, and team communication to save children’s lives.
This blog breaks down PALS Megacodes and scenarios in a clear, step-by-step way. You’ll learn how providers apply American Heart Association–based algorithms, manage common pediatric emergencies, and practice teamwork under pressure. From study tips and real-life examples to avoiding common mistakes, this article equips students, clinicians, and anyone preparing for certification with the knowledge and confidence needed for effective pediatric emergency care.
What Are PALS Megacodes and Why Are They Needed?
A PALS Megacode is a hands-on simulation that trains healthcare providers to handle life-threatening pediatric emergencies. It mimics real situations like cardiac arrest, shock, or severe respiratory distress. Megacodes test a provider’s ability to assess, act quickly, lead a team, and apply PALS guidelines in a realistic, high-pressure environment.
During a Megacode:
- A manikin or standardized patient represents a critically ill child.
- The scenario unfolds in real-time, requiring rapid assessment and intervention.
- Participants are observed and evaluated on clinical skills, decision-making, and teamwork.
Key Takeaway: Megacodes go beyond practice. They give healthcare providers a realistic, safe space to master critical skills and build the confidence needed to respond effectively during real pediatric emergencies.
How Do PALS Megacodes Help Improve Pediatric Emergency Care?
PALS Megacodes train healthcare providers to respond effectively during pediatric emergencies. They simulate real-life scenarios like cardiac arrest, shock, and respiratory distress, giving participants a safe environment to practice assessment, critical decision-making, interventions, and team coordination. These hands-on simulations improve confidence, reduce errors, and prepare providers for real-life emergencies, ultimately saving children’s lives.
Key Points:
Test Emergency Skills
Megacodes give providers hands-on practice with CPR, airway management, and medication administration to build confidence and accuracy in high-pressure pediatric emergencies.Enhance Teamwork
Megacodes train teams to communicate clearly, assign roles, and lead effectively, ensuring safe and coordinated responses during pediatric crises.Identify Knowledge Gaps
Trainers use Megacodes to spot weaknesses in skills, timing, or communication, helping providers improve before real emergencies occur.Improve Patient Outcomes
Practicing in realistic scenarios improves decision-making and reaction time, supporting faster, safer interventions and better survival for children, following American Heart Association guidance.Meet Certification Requirements
Completing Megacodes is often required for PALS certification through the American Heart Association, keeping providers competent and prepared for pediatric emergency care.
What Happens During a PALS Megacode?
A PALS Megacode is a structured simulation that mimics real pediatric emergencies. It allows healthcare providers to practice rapid assessment, decision-making, interventions, and teamwork in a safe environment. Participants experience realistic scenarios, improving skills, confidence, and readiness for real-life pediatric crises.
Events that occur during a PALS Megacode:
1. Pre-Briefing
Before the scenario begins, participants are introduced to objectives, roles, and the simulation environment. This ensures everyone understands their responsibilities, the patient case, and what to focus on, creating a structured and safe learning experience.
2. Scenario Launch
The case starts with initial patient information, vital signs, and presenting complaints. Participants quickly assess the child’s condition and begin interventions, following PALS protocols to stabilize the patient while making critical decisions in real time.
3. Patient Deterioration
As the scenario progresses, the child’s condition may worsen based on the interventions provided. This test participants’ ability to recognize changes, adjust treatment promptly, and apply PALS algorithms under pressure in a realistic, time-sensitive setting.
4. Team Management
Participants must communicate clearly, assign roles, and coordinate interventions as a team. Effective teamwork, leadership, and situational awareness are emphasized to ensure smooth execution of life-saving actions and adherence to PALS guidelines.
5. Scenario Completion
The simulation concludes when the child stabilizes or predefined learning objectives are met. This allows participants to see the impact of their decisions, review clinical outcomes, and understand areas for improvement in a controlled environment.
6. Debriefing
After the scenario, trainers provide structured feedback on both individual and team performance. Strengths, errors, and areas needing improvement are discussed, reinforcing proper techniques and decision-making for real pediatric emergencies.
7. Repeat Scenarios
Participants may engage in additional cases to apply lessons learned. Repeated practice builds skill retention, confidence, and mastery of pediatric emergency management, ensuring healthcare providers are better prepared for a variety of high-pressure situations.
What Pediatric Emergency Scenarios Are Most Commonly Practiced in PALS Megacodes?
PALS Megacodes recreate high-pressure pediatric emergencies so healthcare providers can practice real-life responses safely. These scenarios cover a range of critical conditions, allowing teams to apply PALS protocols, improve teamwork, and gain confidence in responding safely and effectively to high-stakes pediatric emergencies.
Common scenarios practiced during PALS Megacode:
Bradycardia in a Newborn
Providers practice stabilizing a newborn with a low heart rate, applying neonatal PALS protocols to restore normal cardiac function.Anaphylaxis
Healthcare teams learn to quickly identify and treat severe allergic reactions, including administering epinephrine and supportive care.Severe Asthma Attack
Participants manage worsening respiratory distress that does not respond to initial treatment, following PALS respiratory guidelines.Shock
Teams practice recognizing and treating hypovolemic shock after trauma, including fluid resuscitation and monitoring perfusion.Seizure
Providers respond to prolonged febrile seizures in toddlers, ensuring airway safety, seizure control, and timely interventions.Cardiac Arrest
Participants simulate managing pulseless ventricular fibrillation in adolescents, performing high-quality CPR, defibrillation, and advanced life support interventions.
What Key PALS Skills Do Providers Need to Master Before a Megacode?
Before a PALS Megacode, providers must master essential skills to respond quickly and safely. These include rapid assessments, effective teamwork, high-quality CPR, and knowledge of reversible causes. Mastery ensures confident, accurate decision-making during real pediatric emergencies.
Key skills providers need to master before Megacodes:
1. Pediatric Assessment Triangle (PAT)
The PAT is a rapid evaluation tool used to assess a child’s appearance, breathing, and circulation from across the room. It helps providers quickly identify if a child is stable, in distress, or critically ill, guiding immediate interventions.
2. Primary Assessment (ABCDE)
The primary assessment (ABCDE) approach of PALS evaluates Airway, Breathing, Circulation, Disability, and Exposure systematically. This ensures providers identify life-threatening issues quickly, prioritize interventions, and stabilize critically ill children efficiently during high-pressure emergency scenarios.
3. Secondary Assessment (SAMPLE)
The secondary assessment (SAMPLE) in PALS gathers Signs and Symptoms, Allergies, Medications, Past medical history, Last meal, and Events leading to illness. This structured approach helps providers understand the context of the emergency and tailor interventions effectively.
4. High-Quality Pediatric CPR
High-quality CPR focuses on correct compression rate, depth, full chest recoil, and proper ventilation ratios. Mastering these techniques ensures effective circulation and oxygen delivery during cardiac arrest, increasing a child’s chances of survival.
5. Team Dynamics and Effective Communication
Effective team dynamics include assigning clear roles, using closed-loop communication, and maintaining leadership. Strong teamwork ensures tasks are coordinated, errors are minimized, and interventions are delivered efficiently in fast-paced pediatric emergencies.
6. Reversible Causes (Hs & Ts)
Providers must identify treatable causes of cardiac arrest, such as Hypoxia, Hypovolemia, Hydrogen ion imbalance, Hypo/Hyperkalemia, Hypothermia, Tension pneumothorax, Tamponade, Toxins, and Thrombosis. Recognizing these helps target interventions that can reverse life-threatening conditions.
Which PALS Algorithms Are Core for Megacodes?
PALS Megacodes rely on core algorithms to guide rapid assessment and interventions. Mastering these ensures providers respond correctly to cardiac, respiratory, and shock emergencies, improving outcomes in high-pressure pediatric situations.
Here are the core algorithms used in PALS Megacodes:
1. Pediatric BLS Algorithm
The Pediatric Basic Life Support (BLS) Algorithm covers single-rescuer CPR with a 30:2 compression-to-breath ratio and two-rescuer CPR at 15:2. It also includes using an AED promptly. Following this ensures high-quality compressions, effective ventilation, and rapid defibrillation when needed.
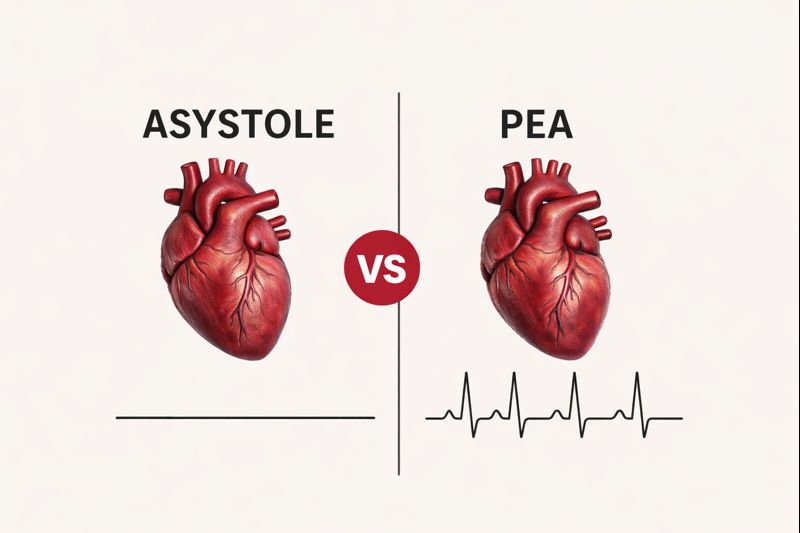
2. Pediatric Cardiac Arrest Algorithm
This algorithm guides providers in managing pediatric cardiac arrest. It includes high-quality CPR, rhythm checks, defibrillation for shockable rhythms, medication administration like epinephrine, and airway management. Following the steps quickly and accurately improves survival rates.
3. Pediatric Tachycardia Algorithm
The Pediatric Tachycardia Algorithm focuses on children with a fast heart rate. It helps determine if the child is stable or unstable, whether the QRS complex is narrow or wide, and guides interventions such as medications or synchronized cardioversion based on the patient’s condition.
4. Pediatric Bradycardia Algorithm
The Pediatric Bradycardia Algorithm addresses children with slow heart rates that may cause poor perfusion. It guides assessment, oxygen support, medication like atropine, and pacing if necessary, ensuring timely treatment to prevent deterioration.
5. Respiratory Distress and Failure Algorithm
This algorithm focuses on managing airway and breathing difficulties. Providers assess the severity of respiratory distress, deliver oxygen, use advanced airway techniques if needed, and intervene quickly to prevent respiratory failure and complications.
6. Pediatric Septic Shock Algorithm
The Pediatric Septic Shock Algorithm helps providers recognize different types of shock, including hypovolemic, septic, or cardiogenic. It guides fluid resuscitation, medications, and supportive care to maintain circulation and oxygen delivery to vital organs.
7. Post-Cardiac Arrest Care Algorithm
After the child achieves Return of Spontaneous Circulation (ROSC), this algorithm ensures ongoing monitoring of vital signs, oxygenation, ventilation, and prevention of secondary injuries, supporting stabilization and recovery.
What Are Common Mistakes During PALS Megacodes?
During PALS Megacodes, learners often make avoidable errors under pressure. Being aware of these mistakes helps providers stay focused, act quickly, and follow protocols correctly, ensuring safer and more effective pediatric emergency care.
Here are the common mistakes during PALS Megacodes:
Delaying CPR Initiation
Waiting too long to start chest compressions slows oxygen delivery and reduces survival chances. Immediate CPR is essential for all pulseless children.Forgetting to Reassess the Patient’s Response
Providers must continuously check vital signs and clinical response after each intervention to adjust care as needed. Reassessment ensures treatments are effective.Administering Incorrect Medication Doses
Giving wrong weight-based doses can harm the patient. Always confirm the child’s weight and follow AHA guidelines for accurate medication administration.Poor Communication or Ignoring Closed-Loop Techniques
Failure to communicate clearly or confirm instructions can create confusion. Using closed-loop communication keeps the team coordinated and improves patient safety.Overlooking Reversible Causes of Cardiac Arrest
Ignoring treatable conditions like hypoxia, hypovolemia, or toxins can delay critical interventions. Always consider the H’s and T’s during resuscitation.Missing Rhythm Changes on Monitors
Changes in heart rhythm may signal deterioration. Providers should monitor continuously to detect and treat new arrhythmias promptly.
How Can You Prepare for and Succeed in PALS Megacode Exams?
Preparing for PALS Megacodes requires practice, focus, and knowledge of key protocols. Learning medications, rhythms, team communication, and stress management helps providers perform confidently and effectively during exams and real-life pediatric emergencies.
Here are the tips for the Megacode exam:
Memorize Key Medications
Learn weight-based drug doses using charts to ensure fast, accurate administration during high-pressure situations, following American Heart Association guidelines.Practice Reading Rhythms
Regularly interpret cardiac rhythms to recognize abnormal patterns quickly, enabling timely interventions during megacode simulations or real emergencies.Run Mental Megacodes
Walk through PALS algorithms step by step in your mind to reinforce decision-making, sequence, and confidence before live scenarios.Use Flashcards for Hs & Ts
Study reversible causes of cardiac arrest, like Hypoxia, Hypovolemia, or Tension pneumothorax, with flashcards for fast recall under pressure.Simulate Stress
Timed practice drills mimic real-life pressure, helping providers remain calm, make quick decisions, and apply correct interventions during megacodes.Practice Team Leadership
Assign roles, communicate clearly, and lead efficiently to ensure the team works together seamlessly and patient care is optimized.
Master PALS Megacodes and Pediatric Emergencies
PALS Megacodes prepare providers to act decisively in high-pressure pediatric crises. Practicing realistic scenarios, mastering PALS protocols, and improving teamwork builds confidence and accuracy. Learning from mistakes, rehearsing interventions, and reinforcing clear communication ensure readiness for both exams and real-life emergencies. Regular practice transforms skills into swift, effective action, giving critically ill children the best chance at survival.
Be ready to save lives with CPR VAM. Our hands-on BLS, ACLS, and PALS courses let you practice critical pediatric interventions through realistic Megacode simulations. Work through real scenarios, strengthen teamwork, and apply American Heart Association protocols under expert guidance. Gain the confidence, skills, and certification you need to act quickly in emergencies. Complete your course and leave prepared for any high-pressure situation.
FAQs
1. How Long Does a PALS Megacode Usually Last?
Most Megacodes run 15 to 30 minutes, simulating real-time emergencies to test assessment, decision-making, and teamwork under pressure.
2. Can Non-Clinical Staff Watch a Megacode?
Yes. Non-medical people can learn by watching the flow and teamwork, but only trained providers are authorized to perform interventions.
3. Are Mannequins the Only Tools Used in Megacodes?
Not always. Some simulations utilize standardized patients to practice communication, leadership, and rapid decision-making in realistic scenarios.
4. What If I Make a Mistake During a Megacode?
Mistakes are part of learning. Trainers provide feedback to help you improve safely and confidently for real emergencies.
5. How Can I Stay Calm Under Pressure?
Focus on one step at a time, breathe steadily, and rely on practiced algorithms. Repetition builds confidence and composure.