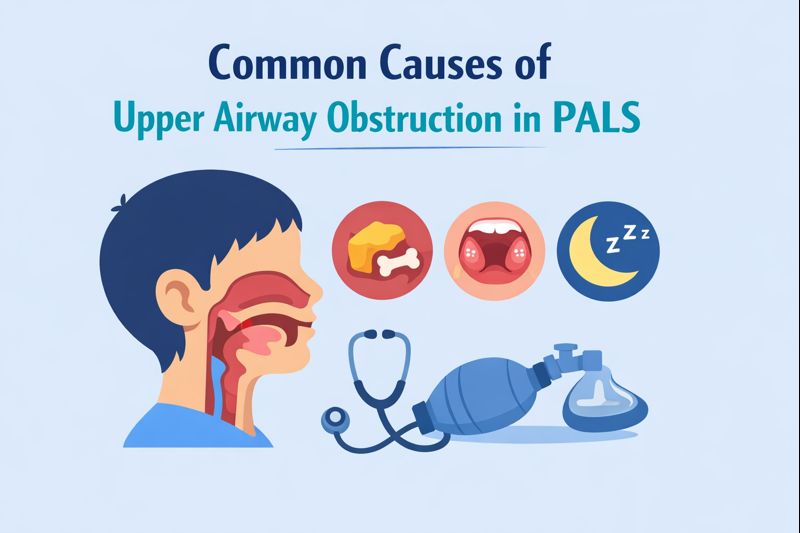
Upper airway obstruction in pediatric patients is a serious and potentially life-threatening condition in Pediatric Advanced Life Support (PALS). It occurs when airflow is partially or completely blocked above the trachea, at the level of the nose, mouth, pharynx, or larynx, preventing adequate ventilation and oxygenation. Because children have naturally smaller and more flexible airways, even minor obstructions can rapidly compromise breathing, making early recognition and intervention critical.
The causes of upper airway obstruction in children are varied, ranging from swelling due to infection or allergic reactions to accumulated secretions and improper airway positioning. Each of these factors can impair airflow quickly, and the clinical presentation can evolve rapidly from mild respiratory distress to severe hypoxia, bradycardia, or cardiac arrest if not addressed immediately. Awareness of the common causes and their mechanisms is essential for timely assessment and effective airway management in PALS.
This blog will explore the common causes of upper airway obstruction in pediatric patients, discuss the signs and symptoms to watch for, and emphasize why immediate intervention is critical in emergencies.
What Is Upper Airway Obstruction in PALS?
Upper airway obstruction in PALS is the partial or complete blockage of airflow above the trachea, specifically at the level of the nose, mouth, pharynx, or larynx, in a pediatric patient. It prevents adequate air movement into the lungs and compromises oxygenation and ventilation.
Within Pediatric Advanced Life Support (PALS), upper airway obstruction is classified as a time-critical condition because pediatric airways are anatomically narrow and easily compromised. Any obstruction at this level can rapidly impair breathing and lead to clinical deterioration, making early identification during airway assessment a top priority in PALS.
What Can Cause Upper Airway Obstruction in Pediatric Patients?
Upper airway obstruction in pediatric patients can result from a variety of conditions that narrow or block airflow at the level of the nose, mouth, pharynx, or larynx. Understanding these causes is essential in PALS, as early identification allows for rapid intervention and prevention of life-threatening complications.
Common causes of upper airway obstruction in PALS are as follows:
1. Airway Swelling
Airway swelling is a common cause of upper airway obstruction in pediatric patients. Inflammation or edema of the pharynx, larynx, or surrounding tissues can narrow the airway, reducing airflow. Because children have naturally smaller airways, even mild swelling can lead to significant obstruction.
Causes include infections, allergic reactions, or inflammatory conditions, all of which can compromise breathing if not recognized and managed promptly.
2. Trauma
Trauma to the face, neck, or jaw can cause upper airway obstruction in pediatric patients. Injuries may lead to swelling, bleeding, or structural damage that narrows or blocks the airway.
Even minor trauma can compromise airflow in children due to their smaller and more flexible airways. Rapid assessment and airway management are critical in PALS to prevent respiratory compromise and further complications.
3. Tongue Obstruction
Tongue obstruction occurs when the tongue falls back and blocks the upper airway, preventing air from reaching the lungs. This is most common in infants, young children, or any child who is unconscious or sedated, as their muscle tone is reduced and the tongue can easily collapse backward.
Because the pediatric airway is naturally smaller, even partial obstruction by the tongue can significantly impair airflow, leading to difficulty breathing and hypoxia if not promptly corrected. Proper positioning of the head and airway maneuvers are often required to relieve this type of obstruction.
4. Foreign Body Obstruction
Foreign body obstruction is a common cause of upper airway obstruction in pediatric patients, especially in infants and toddlers who frequently put objects in their mouths. Small items such as coins, toys, nuts, or pieces of food can become lodged in the airway, blocking airflow partially or completely.
This type of obstruction often occurs suddenly and can rapidly compromise breathing. Because children have smaller airways, even a small object can cause significant blockage, making prompt recognition and immediate intervention essential to prevent respiratory distress, hypoxia, or cardiac arrest.
5. Congenital Abnormalities
Congenital abnormalities are a common cause of upper airway obstruction in PALS. These are structural defects present at birth that can narrow or block the airway, increasing the risk of respiratory compromise. Examples include laryngomalacia, where soft laryngeal tissues collapse inward during breathing; choanal atresia, which blocks the nasal passages; and Pierre Robin sequence, where a small jaw causes the tongue to fall back and obstruct the airway.
Because pediatric airways are small, even partial obstruction can quickly lead to difficulty breathing and low oxygen levels. Early recognition during PALS assessment is essential to guide timely airway interventions and prevent hypoxia or deterioration.
6. Secretions
Secretions can block the upper airway and obstruct in pediatric patients. Mucus, blood, or vomit can accumulate in the mouth, nose, or throat, reducing airflow and making breathing difficult. Because children have smaller airways, even a small amount of secretions can lead to significant obstruction and rapid oxygen desaturation.
During PALS, early identification and prompt removal through suctioning or airway clearing maneuvers are critical to maintain adequate ventilation and prevent respiratory compromise.
7. Airway Malposition
Upper airway obstruction can result when a child’s airway is not properly aligned. Poor positioning of the head, neck, or body may allow the tongue or soft tissues to fall back and block airflow. Because pediatric airways are smaller and more flexible, even minor misalignment can quickly reduce ventilation.
In PALS, correcting airway position through techniques such as head tilt, chin lift, or jaw-thrust is critical to maintain oxygenation and prevent respiratory compromise.
What Are the Signs and Symptoms of Upper Airway Obstruction?
Upper airway obstruction in pediatric patients can develop rapidly, and early recognition is critical during PALS. Some of the common signs and symptoms of upper airway obstruction in pediatric patients include:
Stridor
A high-pitched sound, usually heard during inspiration, indicates partial airway blockage.Noisy Breathing or Snoring
Caused by turbulent airflow through a narrowed airway.Increased Work of Breathing
Retractions (pulling in of chest muscles), nasal flaring, or use of accessory muscles.Cyanosis
Bluish discoloration of the lips, tongue, or skin due to inadequate oxygenation.Difficulty Speaking or Crying
A weak, muffled, or absent voice suggests significant obstruction.Altered Mental Status
Restlessness, lethargy, or decreased responsiveness due to hypoxia.Apnea or Respiratory Arrest
In severe cases, obstruction can stop airflow completely, leading to life-threatening respiratory failure.
Recognizing these signs early allows rapid intervention, such as airway repositioning, suctioning, or advanced airway management, to prevent hypoxia, bradycardia, and cardiac arrest in pediatric patients.
Why Immediate Intervention Is Critical?
Upper airway obstruction in pediatric patients is a time-sensitive emergency. Children are particularly vulnerable because their airways are smaller and more flexible, and they have lower oxygen reserves compared to adults. Even minor obstruction can quickly lead to respiratory compromise, hypoxia, and life-threatening complications. Immediate intervention during PALS is essential to prevent rapid deterioration.
Key reasons why prompt action is critical:
Rapid Hypoxia
Reduced airflow quickly decreases oxygen levels in the blood.Progression to Bradycardia
Low oxygen can slow the heart rate, which may precede cardiac arrest in children.Risk of Cardiac Arrest
Severe or complete airway obstruction can quickly cause respiratory and then cardiac arrest.Brain Injury
Prolonged hypoxia can lead to irreversible neurological damage.Limited Pediatric Oxygen Reserve
Children have smaller functional residual lung volumes, so they desaturate faster than adults.Preventing Further Complications
Early intervention allows airway clearance and management before deterioration becomes severe.
Prompt recognition, airway maneuvers, suctioning, foreign body removal, or advanced airway management are all essential steps to restore ventilation and improve outcomes in pediatric patients.
Get Trained Today to Protect Pediatric Airways Tomorrow
In conclusion, upper airway obstruction in pediatric patients is a life-threatening condition that requires rapid recognition and intervention during PALS. Common causes of upper airway obstruction include airway swelling, tongue obstruction, foreign bodies, congenital abnormalities, and secretions. Early identification of warning signs, such as stridor, increased work of breathing, cyanosis, or altered mental status, and prompt airway management are critical to prevent hypoxia, bradycardia, and cardiac arrest. Because children have smaller, more flexible airways and limited oxygen reserves, timely and effective interventions can be life-saving and are essential to maintaining adequate ventilation and oxygenation.
To be fully prepared to recognize and manage airway emergencies in children, proper training is essential. Join CPR classes with CPR VAM, which provides AHA-approved BLS, ACLS, and PALS courses designed to train healthcare providers and individuals who want to learn life-saving techniques. These courses equip participants with the knowledge, skills, and confidence needed to respond effectively during pediatric emergencies and improve patient outcomes.
FAQs
1. How Do You Know If a Child’s Airway Is in Danger?
Signs like noisy breathing, stridor, or bluish lips indicate the airway may be blocked. Early recognition is critical to prevent oxygen deprivation to vital organs.
2. What Common Factors Can Block a Child’s Airway?
Swelling, tongue collapse, foreign objects, secretions, trauma, and congenital issues often cause airway blockage. Even small obstructions can rapidly compromise a child’s breathing.
3. Which Warning Signals Should Make You Act Instantly?
High-pitched stridor, snoring, chest retractions, nasal flaring, or blue lips are urgent warning signs. Acting immediately can prevent life-threatening complications.
4. Why Can a Blocked Airway Become Critical So Fast in Kids?
Children have smaller lungs and limited oxygen reserves, so blockages can quickly cause low oxygen or a slow heart rate. Prompt action during emergencies prevents brain injury or cardiac arrest.
5. What Quick Fixes Can Save a Child’s Airway During PALS?
Simple steps like proper head positioning, suctioning, or removing an obstruction can restore airflow. If these fail, advanced airway techniques may be needed urgently and are essential.