Learn Pediatric Tachycardia Treatment Algorithm!
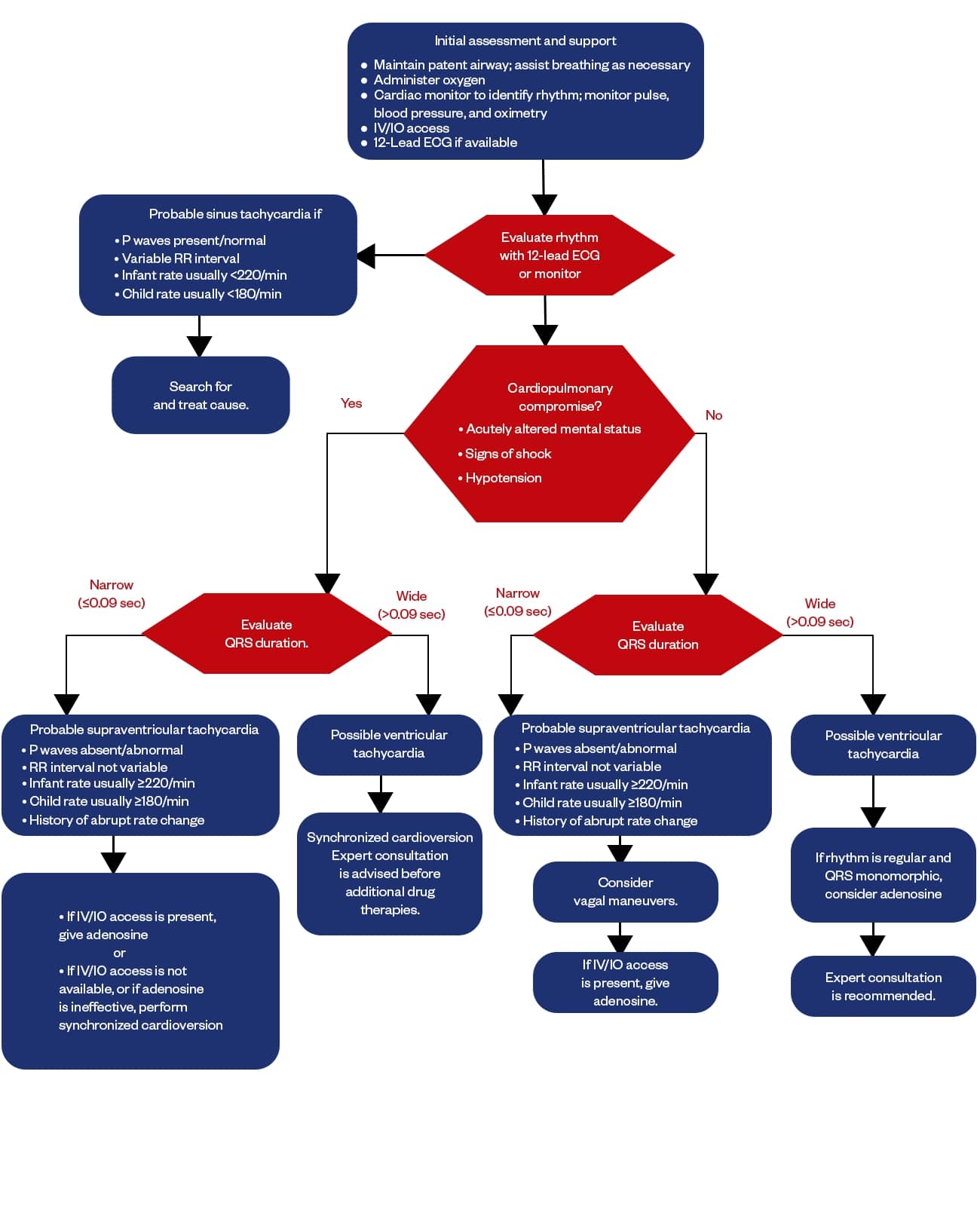
The Pediatric Tachycardia Algorithm is a systematic approach to treating pediatric tachycardic patients. It guides doctors, nurses, specialists and experts involved in the children’s healthcare from basic airway, breathing, circulation (ABC) evaluation to the advanced treatment like adenosine and synchronized cardioversion. It focuses on early initial assessment, immediate medical intervention, and continuous monitoring and support.
Healthcare professionals are required to learn PALS skills and get certified to remain compliant with their work, and even laypeople can hugely benefit by taking the PALS certification. PALS courses equip you with in-depth knowledge and hands-on skills on different treatment algorithms and prepare you to handle real pediatric emergencies confidently. If you are looking for a reliable training center, trust CPR VAM to offer you the comprehensive CPR courses like BLS, PALS, and ACLS.
Enroll today and boost your emergency preparedness!