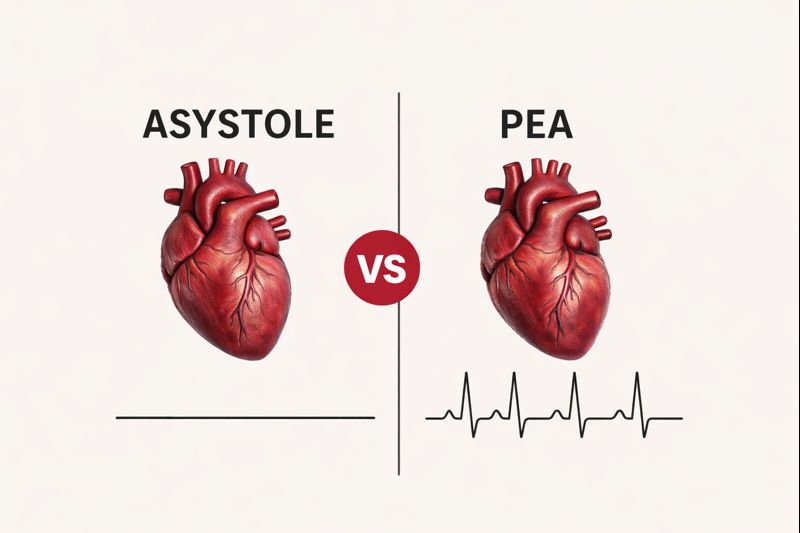
When a person experiences cardiac arrest, fast and accurate rhythm recognition can save lives. Two of the most serious rhythms encountered in these emergencies are Asystole and Pulseless Electrical Activity (PEA). While both are classified as non-shockable rhythms, they are not the same, and confusing them can delay proper treatment.
This blog breaks down asystole vs PEA from a clear, high-level overview to practical clinical differences. Healthcare providers, students, and emergency responders will learn how these rhythms present, why they occur, and how each should be managed according to current resuscitation guidelines.
Why Is It Important to Understand Asystole vs PEA in Cardiac Arrest?
In a cardiac arrest, quick and accurate rhythm recognition guides every lifesaving decision. Asystole and PEA may both be non-shockable, but they require different priorities in care. Knowing the difference helps providers act faster, avoid harmful delays, and focus on the treatments that give patients the best chance of survival.
Identifying the rhythm correctly determines:
- Whether defibrillation is appropriate
- Which medications should be given
- Whether the condition may be reversible
While both asystole and PEA need prompt CPR and epinephrine, PEA often results from reversible conditions that can be treated, whereas asystole typically indicates advanced, life-threatening heart failure.
Recognizing the key differences between asystole and PEA can guide timely treatment, improve decision-making, and significantly increase the chances of survival and positive patient outcomes.
What Does Asystole Mean in Cardiac Arrest?
Asystole occurs when the heart completely stops sending electrical signals. This “Flatline” rhythm means the heart cannot contract or pump blood, making immediate CPR and medical intervention crucial for the patient’s survival. Quick recognition is essential for timely resuscitation.
Asystole is defined by the total absence of electrical activity. On an ECG, it appears as a straight, flat line with no waves or contractions. Clinically, this means no heartbeat, no cardiac output, and no palpable pulse, requiring urgent lifesaving measures.
Heart Activity During Asystole
During asystole, the heart’s entire electrical system fails. The natural pacemakers, including the SA node, AV node, and bundle branches, stop functioning, preventing any electrical impulses, contractions, or blood circulation, making immediate CPR and intervention critical.
Key Highlights
- Sinoatrial (SA) node
- Atrioventricular (AV) node
- Bundle branches
Because there is no electrical activity, defibrillation does not restore a heartbeat. Immediate CPR and medications are necessary.
Causes of Asystole
Asystole typically occurs due to severe or prolonged physiological failures that disrupt the heart’s electrical activity, preventing contractions and circulation, and requiring urgent resuscitation to attempt survival.
- Massive myocardial infarction (Heart attack)
- Prolonged hypoxia (Lack of oxygen)
- Severe trauma or hemorrhage
- Extreme electrolyte imbalances, especially potassium
- Advanced metabolic acidosis
- Prolonged untreated cardiac arrest
Note: Always verify true asystole by examining at least two ECG leads, since loose electrodes or fine ventricular fibrillation can appear similar to a flatline.
How Is Pulseless Electrical Activity (PEA) Defined in Cardiac Arrest?
Pulseless Electrical Activity (PEA) happens when the heart shows electrical activity but fails to pump blood. Despite the rhythm on an ECG, there is no pulse, leaving the patient clinically unresponsive. Immediate intervention is critical.
Recognizing PEA quickly is essential because it often stems from reversible causes. Unlike asystole, PEA may respond if underlying problems are corrected promptly. Timely CPR and treatment targeting the cause significantly improve survival chances in cardiac arrest situations.
Key Features of PEA
PEA is unique because the heart’s electrical system is active, yet mechanical contraction fails. Clinically, there is no pulse or circulation. ECG rhythms may look normal, including sinus rhythm, atrial fibrillation, or junctional rhythms.
Essential Points
- Electrical rhythm is present
- The heart muscle does not contract effectively
- No palpable pulse
- No blood circulation
Common Causes of PEA
PEA is often triggered by reversible conditions, summarized using the reversible cause (H’s and T’s) mnemonic. Early identification and correction of these causes can restore effective circulation and improve patient outcomes in cardiac emergencies.
The H’s:
- Hypovolemia
- Hypoxia
- Hydrogen ion (Acidosis)
- Hypo/Hyperkalemia
- Hypothermia
The T’s:
- Tension pneumothorax
- Cardiac Tamponade
- Toxins
- Thrombosis (Pulmonary or Coronary)
Note: Finding the cause of PEA is essential. Treating the underlying problem can restore the heart’s pumping. Early intervention improves the patient’s chance of survival.
How Do Asystole and PEA Look Different on ECG?
Recognizing the differences between Asystole and PEA on an ECG is critical. Asystole shows no electrical activity, while PEA shows organized rhythms without a pulse. Correct interpretation guides immediate treatment and increases the likelihood of patient recovery.
ECG Characteristics of Asystole
Asystole appears as a flat, straight line on the ECG. There are no P waves, QRS complexes, or T waves. This indicates a complete absence of electrical activity, requiring immediate CPR and urgent medical intervention.
- Flat, straight line
- No P waves
- No QRS complexes
- No T waves
ECG Features of PEA
PEA displays organized electrical activity that may mimic normal rhythms, such as sinus rhythm or atrial fibrillation. Despite this, the heart does not contract, leaving the patient pulseless and clinically unresponsive.
- Organized electrical rhythm
- May resemble normal heart rhythms
- Electrical activity without mechanical response
Note: Always verify a pulse, as electrical signals on the monitor don’t guarantee the heart is actually pumping blood.
What Are the Key Differences Between Asystole and PEA?
Understanding the differences between Asystole and Pulseless Electrical Activity (PEA) is vital for effective cardiac arrest management. These rhythms look similar but have different causes, treatments, and outcomes. Correct identification ensures proper interventions and increases the chance of patient recovery.
Here is the clear comparison of Asystole vs PEA
Feature | Asystole | PEA (Pulseless Electrical Activity) |
ECG Rhythm | Asystole appears as a flatline with no visible electrical activity on the ECG. | PEA shows an organized electrical rhythm that may look normal on the ECG. |
Electrical Activity | In asystole, electrical activity in the heart is completely absent. | In PEA, electrical signals are present but fail to produce a heartbeat. |
Pulse | Asystole always results in the absence of a palpable pulse. | PEA also presents without a palpable pulse despite electrical activity. |
Shockable | Asystole is not a shockable rhythm under ACLS guidelines. | PEA is also classified as a non-shockable rhythm. |
Primary Cause | Asystole usually reflects end-stage cardiac failure or prolonged arrest. | PEA is often caused by reversible conditions (H’s & T’s) |
Treatment Focus | Treatment for asystole centers on high-quality CPR and epinephrine. | PEA treatment includes CPR, epinephrine, and rapid correction of the underlying cause. |
Prognosis | Asystole carries a very poor prognosis in most cases. | PEA has a variable prognosis and may be reversible with timely treatment. |
Why Is Defibrillation Not Used for Asystole or PEA?
Defibrillation is designed to stop chaotic heart rhythms so normal electrical activity can restart. In cardiac arrest, using a shock only helps when disorganized electrical signals are present. In asystole and PEA, defibrillation offers no benefit and delays life-saving care like CPR and medication.
In asystole, there is no electrical activity present, so defibrillation cannot restart the heart or restore blood flow.
In PEA, electrical signals are present, but the heart does not contract, which means defibrillation will not produce a pulse.
Using a shock in either rhythm delays effective treatment, and patient survival depends on high-quality CPR, timely epinephrine, and rapid correction of underlying causes.
What Are the ACLS Treatment Guidelines for Asystole and PEA?
The Advanced Cardiac Life Support (ACLS) guidelines from the American Heart Association outline a clear, step-by-step approach for treating asystole and PEA. Because both are non-shockable rhythms, survival depends on rapid CPR, proper medications, and early identification of reversible causes rather than defibrillation.
Here are the ACLS treatment guidelines for Asystole and PEA as follows:
1. Immediate High-Quality CPR
High-quality CPR is the most critical action for patients in asystole or PEA. When the heart stops pumping, CPR keeps oxygen-rich blood moving to the brain and heart. This helps prevent severe brain damage and maintains vital organ function until circulation can be restored.
According to American Heart Association guidelines, chest compressions should be delivered at a rate of 100-120 per minute and at least two inches deep. Interruptions should be minimal. Consistent, strong compressions improve blood flow to the heart and brain, increasing the likelihood of return of spontaneous circulation (ROSC).
2. Epinephrine Administration
Epinephrine is essential for non-shockable cardiac arrest rhythms. It constricts blood vessels, increasing blood pressure and improving perfusion to the heart and brain. This is crucial when the heart cannot pump effectively on its own.
ACLS recommends 1 mg of epinephrine via IV or IO every 3-5 minutes. It should be administered early and continued throughout resuscitation. Timely dosing, combined with high-quality CPR, improves the chance of restoring circulation and achieving successful resuscitation outcomes.
3. Airway and Ventilation
Providing oxygen and managing the airway are critical to prevent further brain and organ injury. Basic airway techniques, such as a bag-mask device, should be started immediately during CPR to maintain oxygenation.
If trained providers are available, an advanced airway may be placed. Ventilations should be controlled, avoiding excessive breaths. Over-ventilation can increase chest pressure, reducing blood flow back to the heart and lowering the effectiveness of resuscitation.
4. Rhythm Checks Every Two Minutes
Regular rhythm checks determine whether the heart rhythm has changed or circulation has returned. These checks should be performed every two minutes and must be quick to prevent long pauses in chest compressions.
If the rhythm remains asystole or PEA, CPR must resume immediately. Delays during checks can reduce blood flow to vital organs and decrease survival chances. Short, well-organized pauses enhance the overall effectiveness of resuscitation.
5. Identify and Treat Reversible Causes
Finding the underlying cause of cardiac arrest is especially important in PEA, where many conditions are potentially reversible. Correcting these causes can restore effective circulation even when the heart has electrical activity but no pulse.
The H’s and T’s framework guides this process. Conditions like hypoxia, hypovolemia, tension pneumothorax, or cardiac tamponade should be addressed promptly. Treating these underlying problems significantly increases the chances of survival and improves patient outcomes.
What Are Common Mistakes in Recognizing Asystole and PEA?
Even trained healthcare providers can make errors during cardiac arrest, especially under pressure. Misidentifying rhythms or misinterpreting ECG readings can delay correct treatment and reduce survival chances. Awareness of common mistakes helps improve patient outcomes.
Some common mistakes to recognize Asystole and PEA are as follows:
Mistaking PEA for a shockable rhythm, which can lead to unnecessary defibrillation.
Assuming electrical activity automatically means a pulse is present can cause inappropriate treatment.
Misreading artifacts or loose ECG leads as asystole, leading to incorrect intervention.
Attempting defibrillation when CPR is required wastes critical time.
Failing to identify and treat reversible causes, especially in PEA, which may be potentially correctable.
Key Consideration: Accurate assessment of cardiac arrest rhythms requires careful interpretation of the ECG along with manual pulse checks. Relying on only one can lead to misdiagnosis and delayed life-saving treatment.
Asystole and PEA: Essential Insights for Healthcare Providers
Cardiac arrest demands swift, informed action. Knowing the differences between asystole and PEA guides providers to the correct interventions. Immediate CPR, timely epinephrine, and addressing reversible causes can turn a critical situation around. While both rhythms are non-shockable, understanding their unique features reduces treatment errors. Healthcare professionals and emergency responders who recognize these distinctions act faster, make better decisions, and significantly improve patient survival during high-pressure cardiac emergencies.
Gain the confidence to act decisively in life-threatening situations with CPR VAM. Our hands-on, scenario-based ACLS training helps healthcare professionals identify critical rhythms and apply protocols correctly. Whether you’re new to ACLS or renewing certification, join us today to be ready when it matters most.
FAQs About Asystole vs PEA
1. What is the Main Difference Between Asystole and PEA?
Asystole is a flatline with no electrical activity and no heartbeat. Pulseless Electrical Activity has organized electrical signals, but the heart still does not pump, so quick recognition is critical for effective resuscitation.
2. Why Can’t Defibrillation Be Used for Asystole or PEA?
Defibrillators only work for chaotic heart rhythms. In Asystole, there is no electrical activity to reset, and in PEA, the heart has electrical activity but no contractions, giving CPR, epinephrine, and treatment of underlying causes the priority.
3. What Causes PEA, and Can It Be Reversed?
PEA often results from treatable conditions such as hypovolemia, hypoxia, acidosis, potassium imbalances, tension pneumothorax, cardiac tamponade, toxins, or thrombosis. Rapid identification and correction of the cause can sometimes restore effective circulation.
4. How Can Asystole and PEA Be Identified on an ECG?
Asystole shows a flatline with no waves, while PEA displays organized electrical rhythms that may look normal but do not produce a pulse. Always confirm the presence or absence of a pulse along with ECG interpretation.
5. What is the ACLS Treatment Approach for These Rhythms?
Immediate high-quality CPR, timely epinephrine administration, proper airway management, and rhythm checks every two minutes are essential. In PEA, it is also crucial to find and treat the underlying cause, as defibrillation will not help.