Your heart usually beats steadily, keeping blood flowing to your body and brain. But sometimes, a dangerous rhythm called Pulseless Ventricular Tachycardia (pVT) can strike. In PVT, the lower chambers of the heart beat so fast that blood stops moving. Without immediate action, this can cause sudden collapse, cardiac arrest, or even death.
Understanding PVT can save lives. Knowing the signs, learning emergency steps like CPR and defibrillation, and understanding long-term management are critical for patients and families. American Heart Association (AHA) guidelines, evidence-based treatments, and practical advice are presented in clear, simple terms. The goal is for readers to feel informed, confident, and ready to act if PVT ever happens.
This blog explains PVT, its causes, symptoms, treatment, and ways to prevent it.
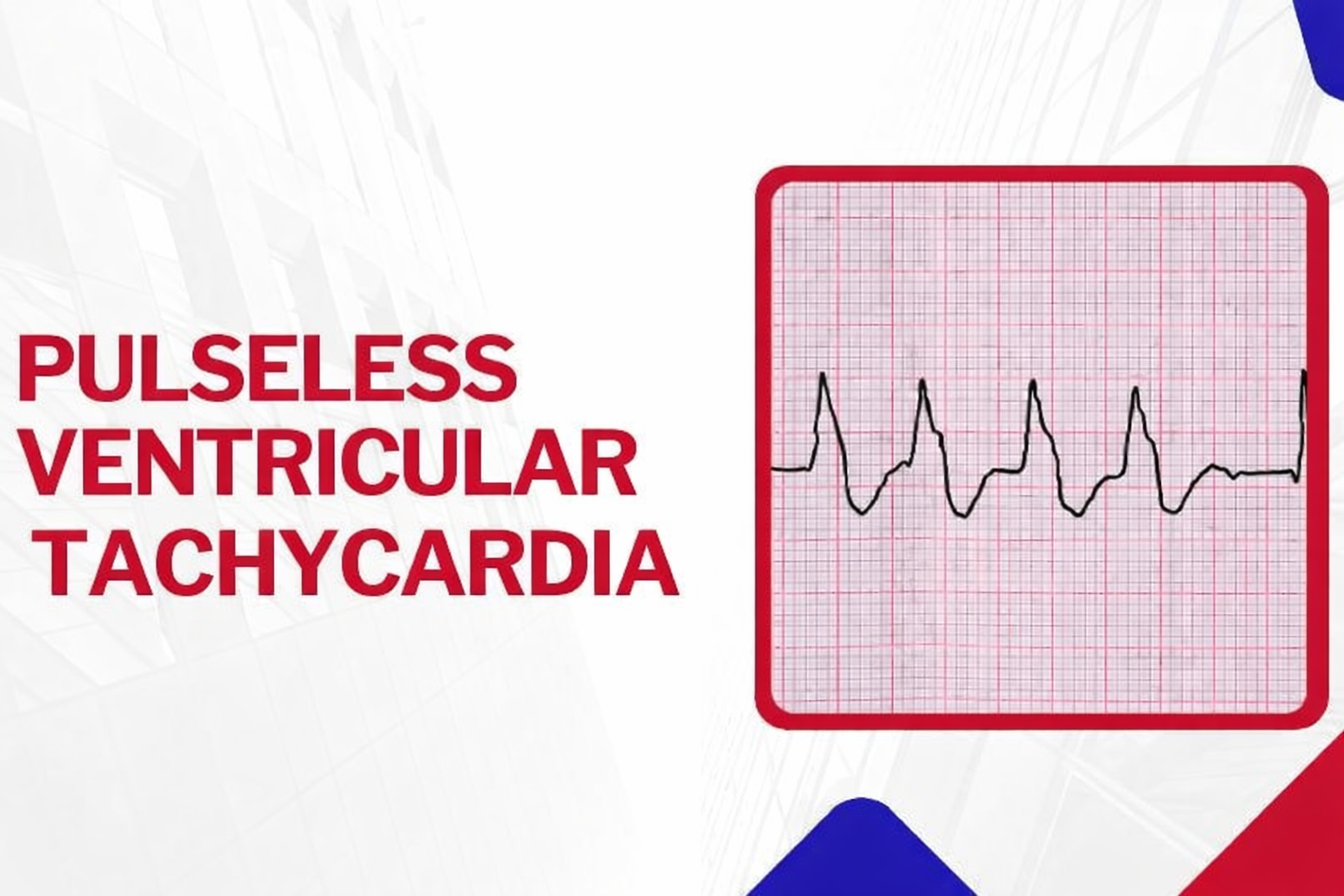
What is Pulseless Ventricular Tachycardia (pVT)?
Pulseless Ventricular Tachycardia (PVT) is a dangerous heart rhythm where the lower chambers beat too quickly to pump blood effectively. Blood circulation stops, causing the pulse to disappear and often leading to sudden collapse or cardiac arrest if not treated immediately.
Some characteristics of pVT
- Rapid heart rate exceeding 100 beats per minute
- Pulse cannot be felt
- The QRS complex may be narrow or wide, based on its origin
- Blood pressure often drops below 80 mmHg
- Risk of losing consciousness if not treated immediately
Immediate action is critical to survival. CPR and defibrillation can restore normal heart rhythm and blood flow. Rapid recognition, emergency response, and hospital care reduce the risk of brain damage, organ failure, and death. Understanding PVT can save lives and improve outcomes.
PVTPulseless Ventricular Tachycardia = Fast Heartbeat + No Blood Flow + Medical Emergency
How Does Pulseless Ventricular Tachycardia Occur?
Pulseless Ventricular Tachycardia (pVT) happens when the heart’s electrical signals in the lower chambers, or ventricles, become abnormal. This causes the ventricles to beat so rapidly that they cannot fill with blood properly.
When the ventricles cannot fill, blood circulation stops. The pulse disappears, oxygen delivery to the brain and organs fails, and the person may collapse suddenly. Immediate medical action, including CPR and defibrillation, is critical to restore blood flow and save a life.
Is Ventricular Tachycardia Always Pulseless?
Ventricular tachycardia (pVT) does not always cause a loss of pulse. In some cases, people remain awake and alert; this is known as stable VT. However, if the heart beats too rapidly, blood cannot circulate. It becomes pulseless VT, a life-threatening form of cardiac arrest. Immediate CPR and defibrillation are required to restore circulation and save life.
What Causes Pulseless Ventricular Tachycardia?
Pulseless ventricular tachycardia occurs when abnormal heart rhythms prevent effective blood flow. It is usually triggered by heart disease, electrolyte imbalances, genetic disorders, or other factors that disrupt normal electrical activity in the heart.
Common Causes Include:
- Previous heart attack
- Heart failure or cardiomyopathy
- Coronary artery disease
- Genetic rhythm disorders such as long QT syndrome
- Electrolyte imbalances, such as low potassium or magnesium
- Drug reactions or stimulant use
- Low oxygen levels
- Severe infections or heart inflammation
Note: In some cases of pulseless ventricular tachycardia, doctors cannot identify a specific trigger. These instances are labeled idiopathic, meaning the cause remains unknown despite thorough evaluation and testing.
What Are the Symptoms of Pulseless Ventricular Tachycardia?
Pulseless ventricular tachycardia can develop suddenly. Early signs include chest discomfort, rapid heartbeat, dizziness, and shortness of breath. Once the condition progresses, the person becomes unconscious, unresponsive, and without a detectable pulse.
Symptoms Before Collapse:
- Chest pain
- Fast or pounding heartbeat
- Dizziness or lightheadedness
- Shortness of breath
Symptoms Once PVT Occurs
- Unconscious
- Unresponsive
- No detectable pulse
When Should You Call Emergency Services?
You should call 911 immediately if someone collapses, stops breathing, or has no pulse. Acting quickly can save a life. If you are trained, begin CPR and use an AED as soon as possible.
Emergency Signs to Watch For:
- Collapses suddenly
- Is not breathing normally
- Has no pulse
- Does not respond
You have to start CPR immediately and use an AED if available to maintain blood flow and restore the heart’s rhythm, increasing the chance of survival.
How Is Pulseless Ventricular Tachycardia Treated?
Pulseless ventricular tachycardia is a life-threatening emergency that needs immediate action. Treatment focuses on restoring a normal heartbeat, maintaining blood flow, and preventing organ damage. Fast and proper intervention can save lives and reduce long-term complications.
Effective treatments for Pulseless Ventricular Tachycardia:
1. Perform Life-Saving CPR
Chest compressions are essential to maintain blood flow to the brain and other vital organs when the heart stops pumping effectively. The American Heart Association (AHA) recommends a rate of 100-120 compressions per minute with a depth of 2-2.4 inches in adults. Immediate action helps prevent permanent damage and increases survival chances.
You should continue compressions without delay until trained help arrives or the heart rhythm is restored. Proper hand placement, depth, and the correct rate improve effectiveness, making CPR a life-saving first step in pulseless ventricular tachycardia emergencies.
2. Quick Defibrillation/ AED Use
Defibrillation delivers an electric shock to the heart, restoring a normal rhythm. Using a defibrillator quickly can dramatically increase survival rates. Timing is critical, so early action is vital while waiting for advanced care.
An automated external defibrillator (AED) can guide you through the process. You should continue CPR alongside defibrillation attempts. Immediate and coordinated use maximizes the likelihood of successfully restarting the heart safely.
3. Provide Key Heart Medications
If the heart rhythm does not stabilize, medications such as Epinephrine, Amiodarone, Lidocaine, Magnesium Sulfate, or Sodium Bicarbonate may be administered. These drugs help support the heart, improve circulation, and increase the chances of successful resuscitation.
Medical professionals carefully monitor dosages and timing to ensure safety. These medications are used alongside CPR and defibrillation, forming a coordinated approach that addresses both the abnormal rhythm and the body’s immediate survival needs.
4. Hospital Care & Monitoring
After emergency treatment, patients are closely observed in a hospital setting. Continuous monitoring checks heart rhythm, organ function, and overall recovery, ensuring that any complications are quickly identified and treated.
Doctors use this period to adjust medications, plan long-term care, and reduce the risk of future episodes. Proper monitoring supports safe recovery and improves overall outcomes for patients who experienced pulseless ventricular tachycardia.
What Long-Term Treatments Help Prevent Recurrence?
Long-term care after pulseless ventricular tachycardia focuses on preventing future episodes. Doctors create personalized plans using devices, medications, or procedures. Managing underlying heart conditions and following medical advice helps reduce risk and improve overall heart health.
Here are the long-term treatments for Pulseless Ventricular Tachycardia:
1. Implantable Cardioverter Defibrillator (ICD)
An ICD is a small device placed under the skin that monitors heart rhythm continuously. If a dangerous rhythm is detected, it delivers an electric shock to restore a normal heartbeat, preventing sudden cardiac arrest. It works automatically without the patient’s effort.
2. Medications
Doctors may prescribe medications to help control heart rhythm and strengthen heart function. Drugs like beta-blockers or antiarrhythmics reduce the chances of dangerous heart rhythms and lower the risk of future life-threatening episodes.
3. Catheter Ablation
Catheter ablation is a procedure where doctors use a thin tube to destroy abnormal electrical pathways in the heart. This helps prevent irregular heartbeats from starting, reducing the risk of dangerous arrhythmias and improving long-term heart stability.
4. Treatment of Underlying Heart Conditions
Addressing conditions such as heart failure, coronary artery disease, or electrolyte imbalances is essential. Proper treatment, lifestyle adjustments, and regular checkups help prevent recurrence of pulseless ventricular tachycardia and improve overall heart health.
Can Pulseless Ventricular Tachycardia Be Prevented?
Pulseless ventricular tachycardia cannot always be prevented. You can lower your risk by taking medications as prescribed and managing heart conditions carefully. Keep your electrolytes balanced and avoid stimulant drugs. Regular heart checkups help detect problems early and protect your heart from dangerous rhythm disturbances.
What Lifestyle Changes Lower the Risk of PVT?
Adopting heart-healthy habits can significantly reduce your risk of pulseless ventricular tachycardia. Simple daily actions like proper diet, regular exercise, and stress management support your heart and overall well-being.
Key Heart-Healthy Habits:
- Eat a balanced diet to support heart function
- Exercise regularly as recommended by your doctor
- Maintain a healthy weight to reduce heart strain
- Quit smoking to improve cardiovascular health
- Limit alcohol and caffeine intake for heart stability
- Manage stress through relaxation techniques and healthy routines
Protect Your Heart and Prevent Pulseless Ventricular Tachycardia Now
Take control of your heart health today. Recognizing pulseless ventricular tachycardia early, acting fast with CPR or an AED, and following long-term medical advice can save lives. Combine this with heart-healthy habits, regular checkups, and careful management of underlying conditions to reduce risk. Staying informed and prepared empowers you to protect yourself and your loved ones while improving overall heart resilience and well-being.
Be ready to save a life! Join the CPR VAM Training Center to master CPR, BLS, ACLS, and PALS. Our AHA-certified courses teach life-saving skills for adults, children, and infants, empowering you to act confidently in pulseless ventricular tachycardia emergencies. Enroll today and make every second count.
FAQs About Pulseless Ventricular Tachycardia
1. How Quickly Can Pulseless Ventricular Tachycardia Become Life-Threatening?
PVT can cause sudden collapse and cardiac arrest within seconds. Immediate CPR and defibrillation are crucial to prevent permanent organ damage or death.
2. Can a Person Survive PVT Without Medical Intervention?
Survival without quick intervention is extremely unlikely. Prompt CPR, use of an AED, and hospital care are essential to restore normal heart rhythm and circulation.
3. How Does an AED Help During a PVT Episode?
An AED delivers an electric shock that can reset the heart’s rhythm. Using it early, alongside CPR, greatly improves survival chances.
4. What Role Do Medications Play in pVT Treatment?
Drugs like epinephrine or amiodarone support the heart and stabilize abnormal rhythms. They are used alongside CPR and defibrillation to increase the likelihood of recovery.
5. Can lifestyle Changes Really Prevent PVT?
Yes. Heart-healthy habits such as regular exercise, a balanced diet, quitting smoking, and controlling stress lower your risk. These changes improve overall heart function and rhythm stability.