When a child stops breathing, every breath truly matters. In such a scary moment, knowing the correct ventilation rate can help save a young life. While chest compressions are a key part of CPR, rescue breathing plays an equally important role, especially in children whose lungs are smaller and more delicate than adults. When you breathe too quickly or too slowly can affect oxygen levels and recovery. That’s why understanding the AHA guidelines for pediatric CPR and the correct ventilation rate for a child in respiratory arrest is so important.
In this blog, we’ll explain how to provide the right number of breaths, why it matters, and how these steps can improve survival during pediatric rescue breathing emergencies.
What is Pediatric Respiratory Arrest?
Pediatric respiratory arrest happens when a child’s breathing either slows down severely or stops completely, leading to a lack of oxygen in the body. When this occurs, the child’s heart and brain don’t receive enough oxygen to function properly. If not treated right away, it can quickly lead to cardiac arrest.
Unlike adults, most cardiac arrests in children start with breathing problems rather than heart issues. This is why recognizing the signs of respiratory arrest early is so important. A child in respiratory arrest may show symptoms such as slow or no breathing, bluish skin color, limp body, or unresponsiveness.
Why Proper Ventilation Rate Matters in Pediatric CPR?
The ventilation rate is one of the most important parts of pediatric CPR. It refers to how often you give rescue breaths to a child who has stopped breathing. During respiratory arrest, a child’s body lacks oxygen, which can quickly lead to brain injury or cardiac arrest if not corrected. Giving the right number of breaths helps maintain oxygen flow to the brain, heart, and vital organs.
Providing the correct ventilation rate matters because:
- Too fast breathing can push air into the stomach instead of the lungs, causing gastric inflation and reducing blood flow to the heart.
- Too slow breathing may not supply enough oxygen, increasing the risk of brain damage or cardiac arrest.
Proper ventilation rate keeps the oxygen and carbon dioxide levels balanced, supporting the body’s natural rhythm. - Following AHA pediatric CPR guidelines ensures each breath is safe, effective, and helps maintain circulation until advanced care arrives.
In simple terms, the right ventilation rate helps rescuers provide quality CPR that truly makes a difference. It’s not just about giving breaths, it’s about delivering them at the right pace and volume to help a child survive and recover safely.
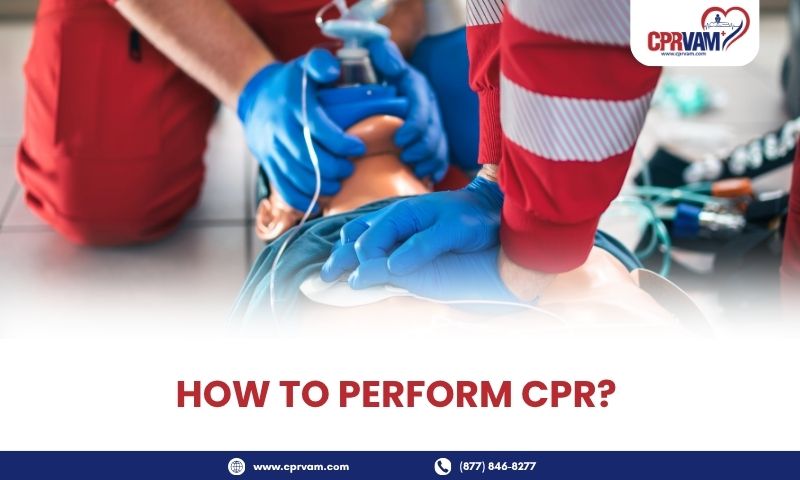
Step-by-Step Guide: How to Provide Rescue Breaths to a Child
It can be challenging to perform rescue breathing on a child, especially in an emergency. If you know the right steps, then you can make it much easier and more effective. Rescue breaths help deliver oxygen to a child’s lungs, which keeps their heart and brain alive until professional help arrives.
Follow these steps carefully:
1. Check Responsiveness and Breathing
The first step in any pediatric emergency is to see if the child is responsive and breathing. Gently tap the child on the shoulder or chest and call their name to check if they react. Look closely for normal breathing, watch the chest for movement, and listen for sounds of breathing. If the child is not responding or is only gasping, this is a sign of respiratory arrest, and you need to act immediately. Recognizing this quickly allows you to start rescue breaths or CPR without delay, giving the child the best chance of survival.
2. Call for Help and Activate Emergency Services
Once you determine that the child is unresponsive and not breathing normally, it’s crucial to get help immediately. Shout for assistance so someone nearby can support you and call emergency services (EMS) right away. If there is an AED (automated external defibrillator) nearby, ask someone to bring it while you begin rescue breaths. Quick activation of emergency services ensures that trained medical professionals arrive as soon as possible, which greatly increases the child’s chances of survival. Acting fast can make the difference between life and serious complications.
3. Open the Airway
After calling for help, the next step is to open the child’s airway so that rescue breaths can be effective. For children, gently tilt the head back slightly and lift the chin to keep the airway clear. For infants under 1 year, use a neutral head position, just a slight tilt so their airway doesn’t get blocked. Opening the airway properly ensures that the air you breathe into the child goes straight into the lungs, rather than the stomach, which makes the rescue breaths more effective and increases the chances of survival.
4. Pinch the Nose and Seal the Mouth
Once the airway is open, it’s important to make a good seal so air goes into the lungs, not outside. This helps each rescue breath be effective and visible through chest rise.
- For Children: Gently pinch the nose shut and cover the mouth completely with your mouth to create a tight seal.
- For Infants: Cover both the mouth and nose with your mouth since their faces are smaller.
This ensures that air enters the lungs properly during each breath.
5. Give rescue breath
After making a proper seal, start giving gentle breaths to help the child’s lungs fill with air. Each breath should be smooth and controlled, not forceful. Watch the chest closely, it should rise with each breath if air is going into the lungs correctly.
- Breathing Rate: Give 1 breath every 2–3 seconds (about 20–30 breaths per minute).
- Breath Duration: Each breath should last about 1 second and make the chest rise visibly.
If the Chest Doesn’t rise: Reposition the head, check the seal, and try again gently.
6. Watch the Chest Rise
As you give each rescue breath, carefully watch the child’s chest to see if it rises. A visible rise means air is entering the lungs properly. If the chest does not rise, it may mean the airway is still blocked or the seal is not tight enough. In that case, reposition the head by tilting it slightly and try another gentle breath. Avoid blowing too hard, as this can push air into the stomach instead of the lungs. Watching the chest rise helps make sure your rescue breaths are effective and safe
7. Continue Rescue Breaths or CPR
If the child still has no pulse or signs of life after giving rescue breaths, you should perform CPR immediately. This means combining chest compressions and rescue breaths following the AHA pediatric CPR guidelines. Continue giving 30 compressions followed by 2 rescue breaths if you are alone, or 15 compressions and 2 breaths if two rescuers are present. You need to keep repeating this cycle until the child starts breathing on their own, shows movement, or emergency medical help arrives. Do not stop unless you are too exhausted or a trained responder takes over.
Common Mistakes to Avoid During Pediatric CPR
Many rescuers make preventable mistakes during pediatric CPR that can reduce a child’s chances of survival. A common error is using adult compression depth or hand placement, which can cause injury or fail to generate enough blood flow. Others include improper compression-to-breath ratios, over-ventilation, or not allowing full chest recoil between compressions. Following the AHA Pediatric Basic Life Support (PBLS) algorithm, rescuers should give compressions at a rate of 100–120 per minute, about one-third the depth of the chest, and ensure smooth coordination if two rescuers are present. When you avoid these mistakes, it improves the quality of CPR and increases the likelihood of successful resuscitation until professional help arrives.
Conclusion
In summary, the correct ventilation rate for pediatric patients in respiratory arrest is vital for maintaining oxygen flow and preventing progression to cardiac arrest. According to AHA Pediatric Basic Life Support (PBLS) guidelines, rescuers should deliver 1 breath every 2–3 seconds, or 12–20 breaths per minute, ensuring visible chest rise without over-inflating the lungs. Consistent, high-quality rescue breathing and CPR can significantly increase survival outcomes for infants and children.
If you’re looking for the best CPR training center near you, trust CPRVAM. We offer life-saving courses, including ACLS, BLS, and PALS, taught by highly qualified instructors who ensure you stay up-to-date with the latest AHA guidelines. Regular pediatric CPR and first aid training equips caregivers, healthcare professionals, and bystanders with the confidence and skills to act swiftly when every second counts.