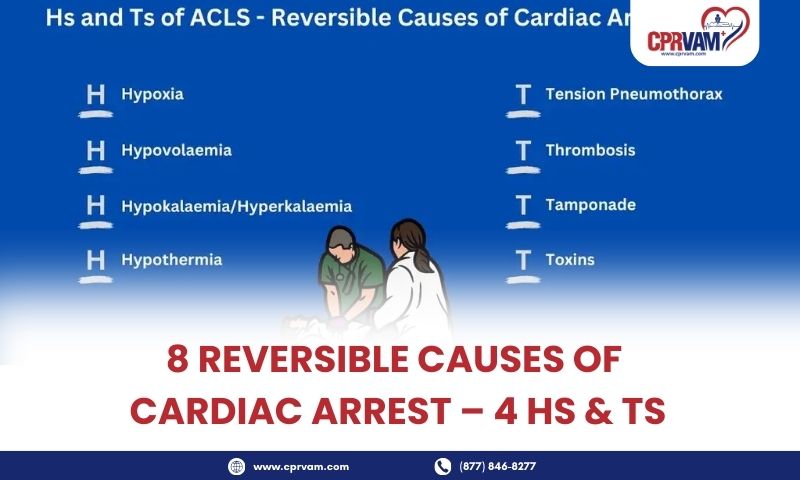
Cardiac arrest is a sudden and life-threatening medical emergency that requires immediate intervention to prevent death or permanent organ damage. While it is often triggered by dangerous heart rhythm disturbances, many cases are caused by underlying, reversible conditions that, if identified and treated quickly, can restore circulation and improve survival outcomes. Medical professionals and first responders rely on a systematic framework known as the 4 Hs and 4 Ts to rapidly recognize and address these life-threatening factors.
The 4 Hs, hypoxia, hypovolemia, hypothermia, and hypo- or hyperkalemia, highlight common metabolic and physiological imbalances that can precipitate cardiac arrest. Meanwhile, the 4 Ts, tension pneumothorax, cardiac tamponade, toxins, and thrombosis, focus on structural, obstructive, and toxic causes that require targeted interventions. Understanding these reversible causes is critical for healthcare providers, as timely recognition and treatment, combined with high-quality CPR and defibrillation, can significantly improve patient survival and neurological recovery.
This article provides a detailed breakdown of each of the 8 reversible causes, their signs and symptoms, common triggers, and evidence-based treatment strategies, equipping healthcare professionals with the knowledge to act decisively during cardiac emergencies.
What is Cardiac Arrest?
Cardiac arrest is a sudden, life-threatening medical emergency in which the heart stops pumping blood effectively. This results in an immediate loss of blood flow to the brain and other vital organs, leading to unconsciousness and, if not treated promptly, death. Unlike a heart attack, which is caused by a blockage in blood flow to the heart muscle, cardiac arrest is primarily a problem with the heart’s electrical system, causing it to beat irregularly or stop altogether.
During cardiac arrest, the body’s tissues and organs are deprived of oxygen, and irreversible damage can occur within minutes. Immediate intervention, including high-quality CPR and defibrillation, is crucial to restore normal heart rhythm and improve the chances of survival. Understanding the underlying causes, particularly reversible conditions like the 4 Hs and 4 Ts, is essential for timely and effective treatment during resuscitation.
What Are the 4 Hs of Cardiac Arrest?
1. Hypoxia (Low Oxygen Levels)
Hypoxia occurs when the body or specific tissues do not receive enough oxygen to function properly. In the context of cardiac arrest, hypoxia can impair the heart’s ability to pump effectively and can be a primary trigger for the arrest.
Common Causes of Hypoxia
- Airway obstruction (e.g., choking, foreign body)
- Respiratory failure (e.g., severe asthma, COPD exacerbation)
- Drowning or near-drowning incidents
- Severe pneumonia or respiratory infections
- Carbon monoxide poisoning
Signs and Symptoms Before Arrest
- Shortness of breath or labored breathing
- Cyanosis (bluish lips or fingertips)
- Confusion or altered mental status
- Rapid heart rate (Tachycardia) initially
Treatment
- Ensure Airway Patency: Clear any obstruction immediately.
- Provide Supplemental Oxygen: Via mask, nasal cannula, or bag-valve-mask ventilation.
- Advanced Airway Management: Endotracheal intubation may be necessary in severe cases.
- Treat Underlying Cause: For example, manage asthma attacks, remove airway obstruction, or treat infections.
Key Point: Hypoxia is one of the most common reversible causes of cardiac arrest. Early recognition and oxygenation are critical to prevent cardiac arrest or improve outcomes during resuscitation.
2. Hypovolemia (Low Blood Volume)
Hypovolemia occurs when there is a significant reduction in circulating blood or fluid volume, leading to inadequate perfusion of organs and tissues. In severe cases, this can trigger cardiac arrest because the heart cannot pump enough blood to sustain life.
Common Causes of Hypovolemia
- Severe Bleeding: Trauma, internal hemorrhage, gastrointestinal bleeding
- Dehydration: From vomiting, diarrhea, or inadequate fluid intake
- Burns: Large fluid losses through damaged skin
- Excessive Fluid Loss: From conditions like severe diuresis or excessive sweating
Signs and Symptoms Before Arrest
- Signs and Symptoms Before Arrest
- Rapid, weak pulse (Tachycardia)
- Low blood pressure (Hypotension)
- Pale, cold, clammy skin, excessive sweating
- Dizziness, confusion, or fainting
- Reduced urine output
Treatment
- Rapid Fluid Resuscitation: Administer intravenous (IV) crystalloids such as normal saline or Ringer’s lactate.
- Blood Transfusion: If there is significant blood loss, transfuse packed red blood cells to restore volume and oxygen-carrying capacity.
- Control Bleeding: Apply direct pressure, use tourniquets if necessary, or perform surgical intervention.
- Treat Underlying Cause: Address the source of fluid loss or hemorrhage to prevent recurrence.
Key Point: Hypovolemia is a reversible cause of cardiac arrest. Prompt recognition and aggressive fluid replacement are critical to restore circulation and improve the chances of survival.
3. Hypo/Hyperkalemia
Hypo/Hyperkalemia refers to abnormal levels of potassium in the blood, either too low (hypokalemia) or too high (hyperkalemia). Potassium is essential for normal electrical activity of the heart, and imbalances can lead to dangerous arrhythmias and cardiac arrest. Other metabolic disorders, like severe acidosis, can also disrupt heart function.
Common Causes
Hypokalemia (Low Potassium)
- Diuretic use (e.g., Furosemide)
- Vomiting or diarrhea
- Excessive sweating
- Certain Endocrine Disorders (e.g., Hyperaldosteronism)
Hyperkalemia (High Potassium)
- Kidney failure or impaired renal function
- Medications like ACE inhibitors, potassium-sparing diuretics
- Massive tissue breakdown (Rhabdomyolysis, burns)
- Acidosis
Signs and Symptoms
- Weakness or muscle cramps
- Fatigue or confusion
- Irregular heartbeat or palpitations
- In severe cases, cardiac arrest may occur suddenly without warning
Treatment
For Hypokalemia
- Potassium Replacement: Oral or intravenous potassium, depending on severity
- Treat Underlying Cause: Address vomiting, diarrhea, or medication-induced loss
For Hyperkalemia
- Stabilize Heart: IV calcium gluconate to protect the heart from arrhythmias
- Shift Potassium Into Cells: Use insulin with glucose, or beta-agonists
- Remove Excess Potassium: Through dialysis, diuretics, or potassium binders
- Treat Underlying Cause: Correct kidney dysfunction or medication effects
Key Point: Electrolyte imbalances are a major reversible cause of cardiac arrest. Rapid identification and correction of potassium abnormalities during resuscitation can restore normal heart rhythm and prevent death.
4. Hypothermia (Low Body Temperature)
Hypothermia occurs when the core body temperature drops below the normal range (usually <35°C or 95°F), impairing normal physiological functions, including the heart’s electrical activity. Severe hypothermia can lead to cardiac arrest because the heart becomes more prone to dangerous arrhythmias.
Common Causes of Hypothermia
- Prolonged exposure to cold environments (e.g., winter outdoors, immersion in cold water)
- Drowning or near-drowning in cold water
- Severe sepsis or shock
- Certain metabolic conditions that impair thermoregulation
Signs and Symptoms Before Cardiac Arrest
- Shivering (May stop in severe cases)
- Slow, weak pulse and low blood pressure
- Pale, cold, and rigid skin
- Confusion, lethargy, or loss of consciousness
- Slow breathing or respiratory failure
Treatment
- Gradual Rewarming: Use warm blankets, heated IV fluids, or external warming devices.
- Warm IV Fluids: Administer warmed crystalloids to help restore core temperature.
- Monitor for Arrhythmias: Hypothermic hearts are very sensitive; handle gently to avoid triggering ventricular fibrillation.
- Treat Underlying Cause: Address exposure, sepsis, or metabolic issues contributing to hypothermia.
Key Point: Hypothermia is a reversible cause of cardiac arrest. Even severely hypothermic patients may survive if core temperature is restored carefully, following the principle: “You’re not dead until you’re warm and dead.”
What Are the 4 Ts of Cardiac Arrest?
1. Tension Pneumothorax
Tension pneumothorax is a life-threatening condition in which air accumulates in the pleural space (the space between the lung and chest wall) under pressure. This compresses the lungs and heart, preventing adequate ventilation and reducing blood return to the heart, which can lead to cardiac arrest.
Common Causes of Tension Pneumothorax
- Chest trauma (Blunt or penetrating)
- Complications from mechanical ventilation
- Spontaneous Pneumothorax in people with lung disease (e.g., COPD, Asthma)
- Medical procedures like central line insertion or lung biopsy
Signs and Symptoms Before Cardiac Arrest
- Severe shortness of breath and rapid breathing
- Sudden chest pain
- Distended neck veins (Jugular Venous Distension)
- Decreased or absent breath sounds on the affected side
- Tracheal deviation away from the affected side (Late sign)
- Low blood pressure and rapid heart rate (Shock)
Treatment
- Immediate Needle Decompression: Insert a large-bore needle or cannula into the second intercostal space at the midclavicular line to relieve pressure.
- Definitive Treatment with Chest Tube (Thoracostomy): Place a chest tube to continuously drain air and allow lung re-expansion.
- Supportive Care: Provide oxygen and monitor vital signs.
- Treat Underlying Cause: Address trauma or procedural complications as needed.
Key Point: Tension pneumothorax is a reversible cause of cardiac arrest. Rapid recognition and immediate decompression can be life-saving, as cardiac arrest can occur within minutes if untreated.
2. Tamponade (Cardiac)
Cardiac tamponade occurs when fluid (blood, pus, or other fluid) accumulates in the pericardial sac surrounding the heart, creating pressure that restricts the heart’s ability to fill and pump effectively. If untreated, this can rapidly lead to cardiac arrest.
Common Causes of Cardiac Tamponade
- Trauma to the chest (blunt or penetrating)
- Rupture of the heart after a myocardial infarction
- Pericarditis (Infection or inflammation of the pericardium)
- Post-cardiac surgery or invasive cardiac procedures
- Cancer or metastatic disease affecting the pericardium
Signs and Symptoms Before Cardiac Arrest
- Beck’s Triad: Low blood pressure (Hypotension), Distended neck veins (Jugular Venous Distension), and Muffled or distant heart sounds
- Rapid, weak pulse (Tachycardia)
- Shortness of breath and difficulty breathing
- Fatigue, confusion, or anxiety
- Pulsus paradoxus (Drop in blood pressure >10 mmHg during inspiration)
Treatment
- Emergency Pericardiocentesis: Needle aspiration of pericardial fluid to relieve pressure on the heart.
- Surgical Intervention (If needed): Pericardial window or open surgery in cases of trauma or recurrent tamponade.
- Supportive Care: Oxygen, IV fluids, and close hemodynamic monitoring.
- Treat Underlying Cause: Control bleeding, treat infection, or manage malignancy as appropriate.
Key Point: Cardiac tamponade is a reversible cause of cardiac arrest. Rapid recognition and immediate drainage of pericardial fluid can restore cardiac output and prevent death.
3. Toxins (Drug Overdose or Poisoning)
Toxins, including drugs or chemical substances, can impair heart function and metabolism, potentially leading to cardiac arrest. These agents may disrupt heart rhythm, depress cardiac contractility, or cause severe metabolic disturbances.
Common Causes of Toxins
- Medications: Beta-blockers, calcium channel blockers, and digoxin, antiarrhythmic drugs in overdose
- Illicit Drugs: Cocaine, amphetamines, or opioids
- Poisons and Toxins: Carbon monoxide, cyanide, or insecticides
- Other Chemicals: Industrial or household chemical exposures
Signs and Symptoms Before Cardiac Arrest
- Altered mental status (Confusion, drowsiness, or coma)
- Abnormal heart rhythm (Bradycardia, tachycardia, or arrhythmias)
- Low blood pressure or shock
- Respiratory depression or difficulty breathing
- Nausea, vomiting, or seizures, depending on the substance
Treatment
- Supportive Care: Ensure airway, breathing, and circulation (ABCs)
Administer oxygen and fluids as needed - Antidotes (If available): Examples, Naloxone for opioid overdose, activated charcoal for certain ingestions, sodium bicarbonate for tricyclic antidepressant toxicity
- Enhanced Elimination: Consider hemodialysis or other detoxification methods for specific toxins
- Monitor and Treat Arrhythmias: Use ACLS protocols to manage life-threatening heart rhythm disturbances
- Treat Underlying Cause: Identify and remove the toxic substance
Key Point: Toxins are a reversible cause of cardiac arrest. Rapid identification, supportive care, and administration of specific antidotes can restore cardiac function and prevent death.
4. Thrombosis (Pulmonary or Coronary)
Thrombosis refers to the formation of blood clots that obstruct blood flow in critical vessels. When clots block the coronary arteries or pulmonary arteries, it can lead to cardiac arrest due to myocardial infarction (heart attack) or pulmonary embolism.
Types and Causes
1. Coronary Thrombosis (Heart Attack)
- Caused by a clot in the coronary arteries that supply the heart muscle
- Often due to rupture of an atherosclerotic plaque
- Leads to Ischemia and potential cardiac arrest
2. Pulmonary Thrombosis (Pulmonary Embolism)
- Caused by a clot traveling to the lungs, usually from deep vein thrombosis (DVT)
- Obstructs blood flow through the lungs, reducing oxygenation and straining the right side of the heart
Signs and Symptoms Before Cardiac Arrest
1. Coronary Thrombosis
- Chest pain or pressure
- Shortness of breath
- Sweating, nausea, or vomiting
- Palpitations or irregular heartbeat
2. Pulmonary Thrombosis
- Sudden shortness of breath
- Sharp chest pain worsens with breathing
- Rapid heart rate (Tachycardia)
- Low blood pressure in massive pulmonary embolism
Treatment
1. Coronary Thrombosis
- Administer oxygen and pain relief (e.g., Nitroglycerin if appropriate)
- Rapid Reperfusion Therapy, such as percutaneous coronary intervention (PCI), or Thrombolytics
- Supportive ACLS measures during cardiac arrest
2. Pulmonary Thrombosis
- Administer Anticoagulants (Heparin)
- Thrombolytic therapy for massive pulmonary embolism
- Supportive care with oxygen and circulatory support
- Surgical or catheter-based clot removal in selected cases
Key Point: Thrombosis is a reversible cause of cardiac arrest. Early recognition and prompt intervention to restore blood flow can save lives and improve outcomes during resuscitation.
Why Is Knowing the 4 Hs and 4 Ts Important in Cardiac Arrest Management?
Understanding the 4 Hs and 4 Ts is crucial in the management of cardiac arrest because they represent reversible causes that, if identified and treated promptly, can dramatically improve survival.
1. Provides a Structured Approach During Emergencies
Cardiac arrest is chaotic and time-sensitive. The 4 Hs (Hypoxia, Hypovolemia, Hypo/Hyperkalemia, Hypothermia) and 4 Ts (Tension pneumothorax, Tamponade, Toxins, Thrombosis) act as a checklist to systematically evaluate potential causes while performing CPR.
2. Increases Survival Chances
Correcting these reversible causes can restore normal heart rhythm and circulation. For example:
- Treating Hypoxia with oxygen can prevent ongoing tissue damage.
- Performing needle decompression for a tension pneumothorax can immediately save a life.
- Administering antidotes for toxins or correcting potassium imbalances can restore cardiac function.
3. Guides Targeted Interventions
Rather than performing random interventions, the 4 Hs and 4 Ts focus resuscitation efforts on evidence-based, reversible factors, ensuring that treatments are effective and timely.
4. Enhances ACLS and Emergency Training
Healthcare providers trained to recognize these causes are better prepared to make rapid decisions under pressure, improving outcomes in hospitals, emergency settings, and even pre-hospital care.
Take Action: Learn to Recognize and Treat Reversible Causes of Cardiac Arrest
The 8 reversible causes of cardiac arrest, known as the 4 Hs and 4 Ts, provide a critical framework for identifying and correcting life-threatening conditions during resuscitation. By systematically evaluating these reversible causes, healthcare providers can target the underlying cause rather than treating cardiac arrest blindly. Rapid recognition and timely intervention for these reversible factors, alongside high-quality CPR and defibrillation, significantly improve survival rates and neurological outcomes, making the 4 Hs and 4 Ts a cornerstone of effective ACLS and emergency cardiac care.
To effectively apply this framework in real-life emergencies, proper training is essential. Mastery of high-quality CPR, rapid cause identification, and targeted interventions can only be achieved through hands-on, scenario-based education. CPR VAM supports healthcare professionals and first responders with American Heart Association (AHA)–certified CPR, BLS, ACLS, and PALS training, ensuring you are prepared to recognize reversible causes, act decisively under pressure, and improve survival outcomes when every second counts.