Have you ever seen a flatline on a heart monitor and wondered what it means? This is Asystole, one of the most serious cardiac emergencies. It occurs when the heart completely stops its electrical activity, stopping blood flow to vital organs. Understanding what asystole is, its causes, and how it appears on an ECG can help you act quickly and potentially save a life.
Recognizing asystole is not just for doctors or paramedics. Anyone trained in CPR can make a difference. From spotting warning signs to following ACLS protocols, early action is crucial.
This blog explains the meaning of asystole, explores its common triggers, shows how it appears on an ECG, and outlines step-by-step ACLS responses so you are prepared in critical situations.
What Happens to the Heart During Asystole?
Asystole is a serious heart condition where the heart completely stops its electrical activity. On an electrocardiogram, it shows as a flatline, meaning there is no heartbeat or signal. Without fast intervention, the heart cannot pump blood, and organs, including the brain, are deprived of oxygen, making immediate action vital.
This condition leads to cardiac arrest and can be fatal within minutes. Recognizing asystole quickly allows responders to follow ACLS algorithms, including CPR and medication, to try to restart the heart. Understanding how the heart normally works and spotting the flatline on an ECG can save lives in emergencies.
How Does the Heart Normally Work?
The heart works like a pump driven by electrical signals. These signals coordinate each heartbeat, ensuring blood flows efficiently to the lungs and body. When this electrical system works properly, the heart beats regularly, supplying oxygen and nutrients to vital organs.
Key Highlights
Electrical Impulse
The sinoatrial (SA) node acts as the heart’s natural pacemaker. It generates electrical signals that start each heartbeat, triggering the heart chambers to contract and maintain a steady rhythm.Atrial Contraction
The upper chambers of the heart, called atria, contract after receiving the electrical signal. This pushes blood into the lower chambers, preparing the heart for the next strong ventricular pump.Ventricular Contraction
The ventricles, or lower chambers, contract next. This sends oxygen-rich blood to the body and deoxygenated blood to the lungs, ensuring vital organs and tissues receive life-sustaining oxygen.Relaxation (Diastole)
After each heartbeat, the heart relaxes during diastole. This allows chambers to refill with blood, preparing the heart for the next contraction, maintaining continuous and efficient circulation throughout the body.
In asystole, the heart’s electrical system stops working entirely, preventing the chambers from contracting. Without these contractions, blood cannot circulate to the brain and body, creating a life-threatening emergency.
What Factors Lead to Asystole in the Heart?
Asystole occurs when the heart stops generating electrical activity, often due to serious medical problems or emergencies. Identifying the underlying causes quickly is crucial, as some factors are reversible causes (Hs and Ts) with immediate intervention, improving the chances of survival.
1. The Hs: Reversible Causes of Asystole
Hypoxia: When the blood does not carry enough oxygen, the heart cannot function properly, leading to asystole.
Hypovolemia: Severe loss of blood or fluids reduces circulation, which can stop the heart from beating.
Hydrogen Ion (Acidosis): Excess acid in the blood interferes with the heart’s electrical activity, causing cardiac arrest.
Hypo-/Hyperkalemia: Too little or too much potassium disrupts heart rhythm, increasing the risk of asystole.
Hypothermia: Extremely low body temperature slows the heart and may stop electrical activity entirely.
2. Life-Threatening Ts Causes of Asystole
Tension Pneumothorax: Air trapped in the chest puts pressure on the heart, preventing it from pumping effectively.
Cardiac Tamponade: Fluid buildup around the heart restricts its movement and reduces blood flow.
Toxins: Poisoning or drug overdose can interfere with the heart’s electrical system, leading to asystole.
Thrombosis: Blood clots in the heart or lungs block circulation and can stop the heart from beating.
3. Additional Factors That Can Cause Asystole
Severe Heart Disease or Major Heart Attacks: Serious heart conditions can damage the heart muscle and stop its electrical activity.
Serious Infections such as Sepsis: Life-threatening infections can overwhelm the body and disrupt heart function.
Trauma, Drowning, or Electrocution: Physical injuries, lack of oxygen, or electric shocks can trigger the heart to stop.
Metabolic Imbalances, Including Very High or Low Blood Sugar: Extreme changes in blood sugar can interfere with the heart’s rhythm and function.
Asystole often occurs as the final stage of heart failure, sometimes developing after untreated Ventricular Fibrillation (VF) or Pulseless Ventricular Tachycardia (pVT), when the heart’s electrical activity weakens completely and can no longer sustain a heartbeat.
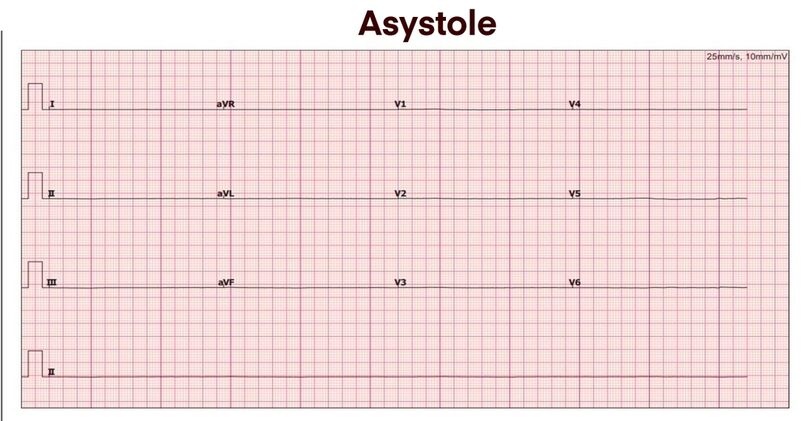
How Can You Identify Asystole on an ECG?
You can identify asystole on an ECG when the monitor shows a flat or nearly flat line, meaning no electrical activity. It confirms the heart has stopped signaling. Always check the patient and ECG leads to avoid false readings.
Key Considerations
Ventricular Fibrillation (VFib)
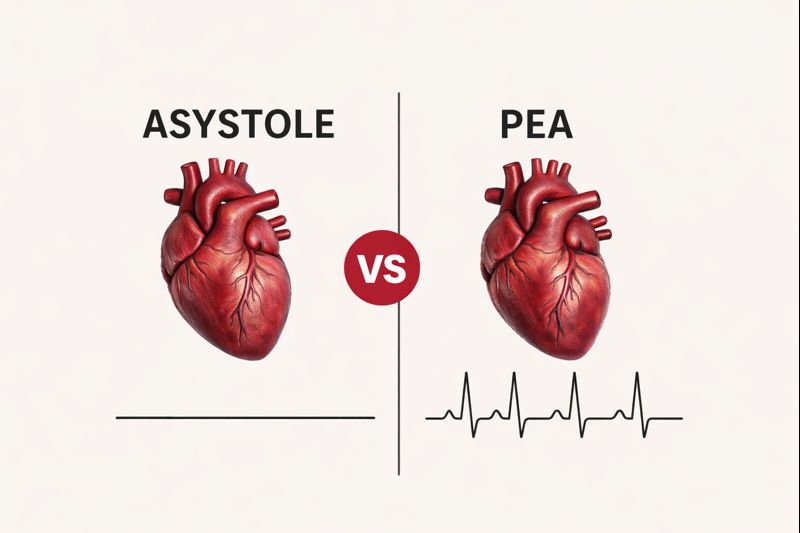
Ventricular fibrillation shows chaotic and irregular waves on the ECG. Although the heart quivers instead of pumping, you can treat VFib with defibrillation and immediate CPR.Pulseless Electrical Activity (PEA)
In pulseless electrical activity, the ECG shows organized electrical signals, but the heart does not pump blood. You cannot shock PEA, so CPR and treating underlying causes are essential.Flatline (Asystole)
Asystole appears as a flatline with no electrical activity at all. You cannot shock this rhythm, so you must start high-quality CPR and follow ACLS protocols immediately.
Note: Always check multiple ECG leads when asystole appears to confirm the rhythm and rule out technical problems, such as loose electrodes, poor contact, or monitor issues, before starting or continuing emergency treatment.
What Immediate ACLS Actions Are Required for Asystole?
When asystole occurs, the heart has no electrical activity, and blood flow stops. According to the American Heart Association ACLS guidelines, you must act immediately. Fast, organized care helps maintain circulation, treat reversible causes, and gives the best chance for return of spontaneous circulation (ROSC).
Here are the immediate ACLS actions that are required to respond to the Asystole as follows:
1. Start High Quality CPR Immediately
High-quality CPR is the most important first step when asystole is detected. You should begin chest compressions immediately to maintain blood flow to the brain and heart. Push firmly and allow full chest recoil to optimize circulation.
Consistent compressions help sustain oxygen delivery while medications and airway management are prepared. You should minimize interruptions and maintain a steady rhythm. Early, effective CPR significantly increases the chance of restoring circulation and protecting vital organs during cardiac arrest situations.
2. Administer Epinephrine at Recommended Intervals
Epinephrine is recommended early in asystole management to improve circulation. You should administer it every three to five minutes while continuing CPR, following ACLS timing. This medication enhances blood flow to the heart and brain, supporting resuscitation efforts.
Although epinephrine does not restart the heart directly, it increases vascular resistance and coronary perfusion. You should continue CPR while administering it and focus on correcting underlying causes. Timely dosing can improve the chances of return of spontaneous circulation when combined with high-quality resuscitation.
3. Manage the Airway and Provide Ventilation
Proper airway management ensures oxygen reaches the lungs and bloodstream. You may begin with bag-valve-mask ventilation and transition to advanced airway placement if trained. You should give controlled breaths at the correct rate to avoid overinflation and support circulation.
Oxygen delivery during resuscitation is critical to protecting the brain and heart. You should coordinate ventilation with chest compressions to maximize efficiency. Maintaining oxygenation helps sustain organ function and supports other ACLS interventions during prolonged cardiac arrest.
4. Identify and Treat Reversible Causes
Asystole often results from conditions that can be corrected. You should actively assess for the Hs and Ts during CPR and medication administration. Identifying hypoxia, hypovolemia, or electrolyte imbalances can be lifesaving when treated promptly.
Correcting reversible causes such as cardiac tamponade, severe blood loss, or toxins may allow the heart’s electrical activity to return. You should continually reassess the patient while addressing these underlying issues, as early treatment increases the likelihood of successful resuscitation.
5. Avoid Defibrillation in Asystole
Asystole is a non-shockable rhythm, meaning defibrillation is not effective. You should not attempt to shock the heart because there is no electrical activity to reset. Focus should remain on CPR, medications, and correcting reversible causes.
Defibrillation is only indicated for Ventricular Fibrillation or Pulseless Ventricular Tachycardia. You should maintain consistent compressions and follow ACLS protocols. Avoiding unnecessary shocks ensures that your resuscitation efforts are targeted and effective, maximizing the patient’s survival potential.
6. Reassess the Patient Continuously
Continuous reassessment is vital during asystole management. You should check the ECG rhythm about every two minutes and monitor for signs of return of spontaneous circulation. This allows you to adapt your interventions quickly and accurately.
Monitoring the patient also helps guide decisions regarding ongoing resuscitation. You should be alert for rhythm changes or improvement. Prompt reassessment ensures that you provide timely interventions and can adjust care according to ACLS guidelines and patient response.
7. Consider Termination of Resuscitation When Appropriate
If the patient does not respond after complete ACLS treatment, termination may be considered. You should evaluate the patient’s response, duration of resuscitation, and overall clinical situation. High-quality CPR and reversible causes must be addressed before considering stopping.
Termination decisions must follow physician guidance and local protocols. You should ensure that all interventions were performed properly. Making this decision carefully balances patient safety, ethical considerations, and the realistic potential for survival following prolonged asystole.
What Are the Survival Chances for Asystole?
Survival chances for asystole are generally low because it usually occurs during severe medical emergencies. You should know that rapid recognition and immediate intervention are crucial, as each minute without CPR significantly reduces the chances of saving a life.
Survival chances in asystole depend on:
Time to Intervention
The sooner CPR is started, the better the chances of survival. You should begin chest compressions immediately, because every minute without intervention decreases the likelihood of return of spontaneous circulation and increases the risk of brain damage.Patient’s Underlying Health
Survival also depends on the patient’s overall health. You should consider that severe heart disease, systemic illnesses, or advanced age can lower the success rates of resuscitation efforts during asystole.Quality of ACLS and CPR
Effective resuscitation improves outcomes. You should ensure that high-quality CPR and ACLS interventions are provided, including proper medication timing, airway management, and correction of reversible causes to maximize the chance of recovery.
Fast recognition of asystole and prompt action, including starting high-quality CPR and following ACLS protocols, can improve the patient’s chance of survival, but overall outcomes remain poor compared to other shockable cardiac arrest rhythms.
Take Action to Improve Survival Chances in Asystole
Asystole is a life-threatening cardiac emergency, but your quick response can make a difference. Recognize the flatline, start high-quality CPR immediately, and follow ACLS protocols. Administer epinephrine, manage the airway, and treat reversible causes to support circulation. Early intervention, consistent care, and knowledge of proper procedures can improve survival, even in severe cases. Staying prepared and acting fast increases the chances of saving a life during this critical cardiac arrest.
Staying current with ACLS training ensures you can act quickly and confidently during cardiac emergencies. CPR VAM’s ACLS courses provide hands-on practice with skilled instructors, giving you the knowledge and skills to save lives. Start your training today and be prepared for any situation.
FAQs About Asystole
1. Can Asystole Be Reversed?
Yes. Asystole can sometimes be reversed with immediate CPR, epinephrine, and treatment of reversible causes. Quick, coordinated action gives the best chance to restore the heart’s activity.
2. Is Asystole Shockable With a Defibrillator?
No. Asystole is a non-shockable rhythm and cannot be treated with defibrillation. CPR and addressing underlying causes are the main ways to attempt resuscitation.
3. How Quickly Should Treatment Start?
Treatment must begin immediately once asystole is recognized. Every minute of delay drastically lowers survival chances and increases the risk of brain damage.
4. Can Young People Experience Asystole?
Yes. Asystole can occur at any age due to trauma, drowning, drug overdose, or congenital heart conditions. Awareness and CPR knowledge are crucial for saving lives in these cases.
5. What Role Do Bystanders Play in Asystole Emergencies?
Bystanders trained in CPR can help maintain blood flow before professional help arrives. Early action, including chest compressions and calling 911, significantly improves survival odds.