Sudden cardiac arrest is a life-threatening emergency that can occur without warning, affecting people of all ages and backgrounds. In these critical moments, immediate action is essential to restore the heart’s normal rhythm and maintain blood flow to vital organs. An Automated External Defibrillator (AED) is one of the most effective tools available for responding to cardiac arrest, especially when used quickly alongside high-quality CPR.
AEDs are increasingly available in public and workplace settings and are designed to be used by everyday individuals, not just healthcare professionals. With clear voice prompts and visual instructions, these devices guide rescuers through each step, making it possible to deliver potentially life-saving defibrillation within minutes. Understanding when and how to use an AED can significantly improve survival outcomes and reduce the risk of long-term complications.
This blog provides a clear, step-by-step guide on how to use an AED, along with important safety precautions, common locations, and myths, to help you respond confidently during a cardiac emergency.
What Is an Automated External Defibrillator (AED)?
An Automated External Defibrillator (AED) is a portable medical device used to help someone experiencing sudden cardiac arrest (SCA). It works by analyzing the heart’s electrical activity and determining whether an electric shock is needed to restore a normal heart rhythm. The shock, known as defibrillation, can be life-saving when delivered quickly, especially in the first few minutes after cardiac arrest.
AEDs are designed to be simple, safe, and effective for public use, even by individuals without medical training. The device provides clear voice and visual prompts that guide users through each step, including pad placement and shock delivery. An AED will only administer a shock if a dangerous heart rhythm is detected, which makes it a reliable and safe tool in emergencies.
When Should You Use an AED?
You should use an AED (Automated External Defibrillator) when someone is experiencing a sudden cardiac arrest. This is a medical emergency where the heart suddenly stops beating effectively, and immediate action is critical.
Signs That an AED Should Be Used
1. Unresponsiveness – The person does not wake up or respond when you tap their shoulder or call their name.
2. Abnormal or Absent Breathing – The person is not breathing normally or is only gasping.
3. No Detectable Pulse – If you are trained to check, the person has no heartbeat.
Important: If you are unsure whether the person is in cardiac arrest, turn on the AED anyway. The device will analyze the heart rhythm and only deliver a shock if needed, so using it is safer than doing nothing.
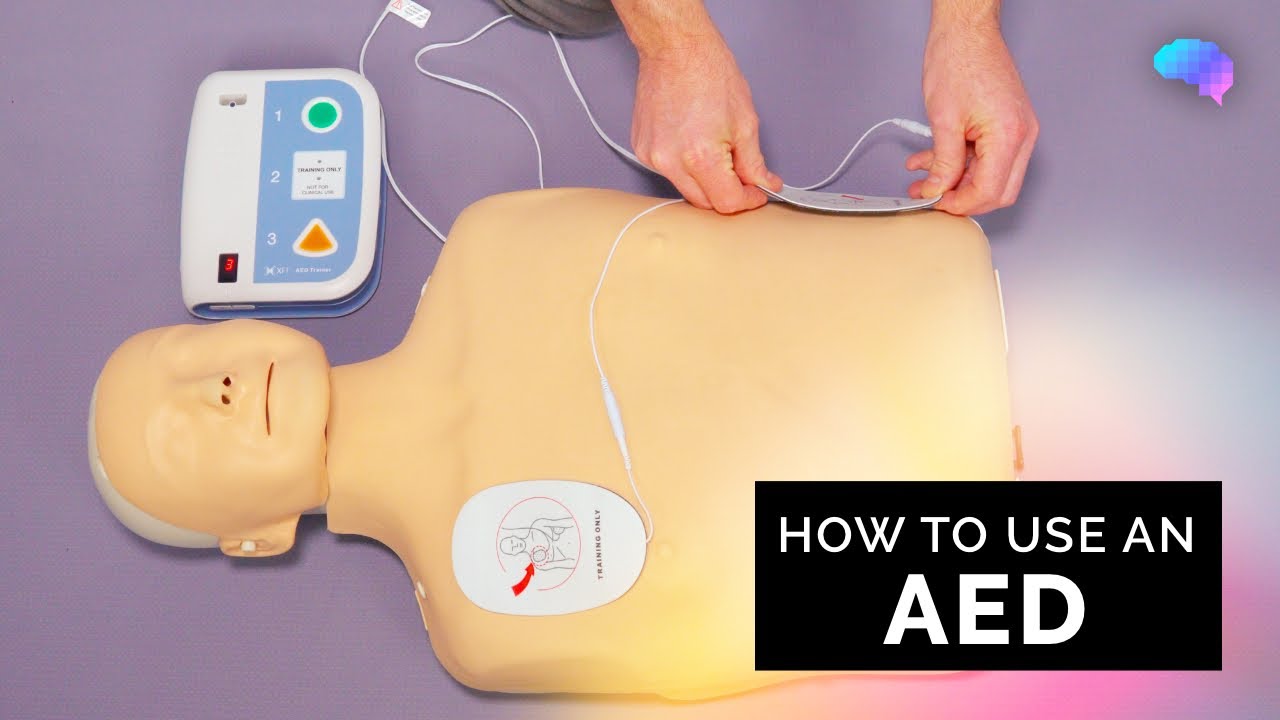
What Are the Steps for Using an AED?
AEDs are designed to be used by the general public, and most devices provide voice prompts and visual instructions to guide users. Following these steps carefully can save a life during sudden cardiac arrest.
Step 1: Check the Patient and Call for Help
If a person collapses suddenly, check for responsiveness, breathing, and pulse.
If the person is unresponsive, not breathing, and pulseless, they are likely experiencing sudden cardiac arrest (SCA).
Call emergency services immediately and explain the situation.
Ask someone nearby to bring an AED.
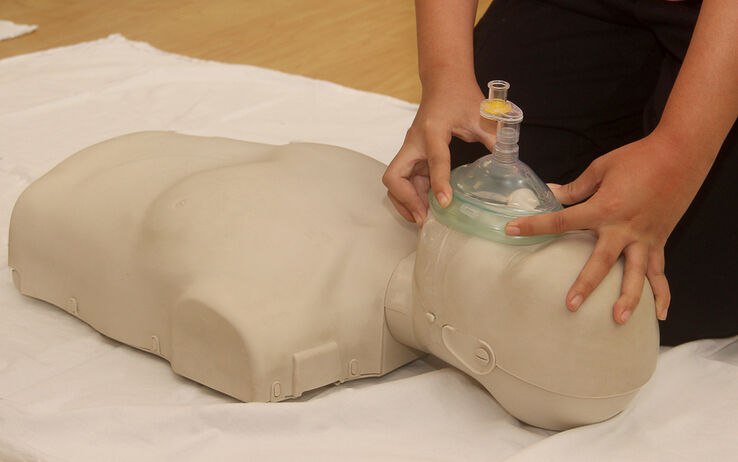
While waiting for the AED, begin CPR to temporarily pump blood to the brain and vital organs.
Step 2: Turn On the AED
When the AED arrives, turn it on and ensure it is functioning correctly.
Follow the audio and visual prompts provided by the device.
Step 3: Prepare the Chest and Attach AED Pads
Remove clothing covering the chest.
If the person is wearing medication patches, remove them carefully with gloved hands if possible.
Wipe the chest dry.
A. Pad Placement for Adults:
Right Pad: upper right chest, just below the collarbone.
Left Pad: lower left chest, several inches below the armpit (anterolateral) placement.
B. Pad Placement for Children (under 8 years or <55 lbs):
Anterior Pad: the middle point of the line connecting the nipples.
Posterior Pad: on the back, opposite side of the anterior pad (anterior-posterior placement.
Remember to plug in the connector if required and ensure pads are secure.
Step 4: Analyze the Heart Rhythm
Once the pads are attached, keep your hands off the patient.
The AED will automatically analyze the heart rhythm to determine if a shock is needed.
Step 5: Deliver a Shock (If Advised)
If the AED indicates a shock:
Fully Automatic AED: This type of AED will deliver the shock automatically after ensuring everyone is clear.
Semi-Automatic AED: For this type of AED, you must press the shock button while ensuring no one is touching the patient.Make sure everyone is standing clear before delivering the shock.
Step 6: Perform CPR
After the shock, immediately resume CPR for 2 minutes
Continue to follow the AED prompts. The device will re-analyze the heart rhythm and advise whether another shock is needed.
Repeat CPR and shocks as necessary until the person shows signs of life (breathing, coughing, moving), or emergency personnel arrive.
Keep the AED pads attached until medical professionals take over.
What Are the Precautions for the Use of AED Devices?
Using an AED can save a life during sudden cardiac arrest, but it is important to follow certain safety precautions. Proper use ensures the device works effectively and protects both the patient and those nearby.
The patient’s chest should be dry and free from sweat or moisture before placing the pads. Avoid using alcohol or other flammable liquids, as the shock from the AED could ignite them.
Do not touch the patient while the AED is delivering a shock. Ensure everyone nearby stays clear to maintain the effectiveness of the defibrillation.
Avoid moving or handling the patient while the AED is analyzing the heart rhythm, as this can interfere with the device’s accuracy.
Keep mobile phones, radios, and other electronic devices at least six feet away to prevent interference with the AED.
Do not operate the AED on wet, metallic, or conductive surfaces, as the electric current could travel to bystanders.
For children under 8 years old or weighing less than 55 pounds, switch to child mode and use pediatric pads if available, as lower-energy shocks are safer.
Remove any medication patches, such as nitroglycerine patches, that may interfere with pad placement or shock delivery.
Keep the AED pads attached and follow all prompts until emergency personnel arrive, even if the patient shows signs of life.
Where Are AEDs Commonly Located?
AEDs are widely available in public spaces to ensure quick access during sudden cardiac emergencies. Knowing where to find an AED can make a critical difference in saving a life. They are usually placed in locations that are easily accessible and highly visible to the public.
Many airports, train stations, and bus terminals have AEDs near main entrances, ticket counters, or waiting areas.
Shopping malls, supermarkets, and large retail stores often place AEDs close to customer service desks or main corridors.
Schools, colleges, and universities typically keep AEDs in gyms, cafeterias, and administrative offices.
Sports arenas, stadiums, and fitness centers have AEDs near locker rooms, main entrances, and seating areas.
Workplaces and office buildings commonly place AEDs in lobbies, break rooms, or near elevators.
Hotels and convention centers usually keep AEDs in lobbies, conference halls, and near emergency exits.
Hospitals and healthcare facilities have AEDs in waiting areas, hallways, and near emergency departments.
Public government buildings, libraries, and community centers often have AEDs at reception desks or main corridors.
AEDs are strategically placed to be accessible within minutes of an emergency, making it easier for bystanders to respond quickly during sudden cardiac arrest.
What Are the Common Myths About AEDs?
Despite their life-saving potential, there are many misconceptions about AEDs that can prevent people from using them effectively in emergencies. Understanding and debunking these myths is essential for encouraging timely action.
Below are some of the myths and their truths about AEDs:
Myth 1: Only medical professionals can use an AED
AEDs are designed for public use and provide voice and visual prompts that guide anyone, even without medical training, through the entire process.
Myth 2: Using an AED can harm the patient
AEDs are safe to use on anyone experiencing sudden cardiac arrest. Following the instructions ensures the shock is delivered only when necessary, minimizing any risk of harm.
Myth 3: AEDs are complicated and hard to operate
Modern AEDs are highly intuitive. The devices use simple step-by-step voice and visual instructions, making them easy for even a first-time user to operate effectively.
Myth 4: AEDs should only be used in hospitals
AEDs are meant to be accessible wherever people gather. Public spaces, offices, schools, and sports facilities are all ideal locations for AED placement.
Myth 5: AEDs are dangerous around children
AEDs are safe for children. Many devices include child mode or pediatric pads to deliver lower-energy shocks specifically designed for younger patients.
Myth 6: CPR alone is enough
While CPR helps maintain blood flow, combining it with an AED significantly increases survival rates in sudden cardiac arrest. AEDs restore normal heart rhythm, which CPR alone cannot do.
Tip: Don’t hesitate to use an AED during an emergency. The device is designed to guide you safely, and early use can save a life.
Learn CPR and AED Skills to Save Lives Today
In conclusion, knowing how to use an Automated External Defibrillator is a critical life-saving skill that can make a decisive difference during sudden cardiac arrest. AEDs are safe, easy to use, and designed to guide bystanders through every step, from assessing the patient to delivering a shock and performing CPR. When used promptly alongside high-quality CPR, an AED can significantly increase survival chances. Understanding when and how to use an AED, following proper precautions, and overcoming common myths empowers individuals to act confidently and effectively in emergencies, potentially saving lives when every second counts.
To enhance your life-saving skills, join CPR VAM for hands-on training in ACLS, BLS, and PALS courses near you. Learn CPR and AED use from experienced instructors, gain confidence in emergencies, and be ready to act when every second matters. Getting trained today could help you save a life tomorrow. Investing in this training ensures you are prepared to make a real difference in critical situations.
FAQs
1. How Long Can An AED Battery Last, And How Do I Know When It Needs Replacing?
AED batteries typically last 2–5 years, depending on the model and frequency of use. Most AEDs have a status indicator or self-test system that alerts you when the battery is low. Regularly checking the AED ensures it’s ready during an emergency.
2. Can AEDs Be Used On People With Implanted Medical Devices Like Pacemakers Or Defibrillators?
Yes, AEDs can be safely used on individuals with pacemakers or implantable defibrillators. Make sure to place the AED pads at least 1 inch away from the implanted device. The AED will still analyze the heart rhythm and deliver a shock if necessary.
3. Are AEDs Effective On Wet Or Icy Surfaces?
AEDs should not be used on conductive surfaces like wet floors or metal. If the person is wet, quickly dry their chest before attaching the pads. If they are on ice, move them to a dry surface if possible. This prevents the shock from traveling to bystanders.
4. How Often Should AEDs Be Maintained Or Tested?
AEDs should undergo monthly inspections for battery life, pad condition, and device readiness. Many AEDs also perform automatic daily or weekly self-tests. Following maintenance schedules ensures the device works correctly when needed.
5. Can An AED Be Used During Pregnancy?
Yes, AEDs are safe for pregnant individuals. Sudden cardiac arrest is life-threatening, and defibrillation can save both the mother and the baby. Apply the pads and follow standard CPR guidelines as usual.