Cardiac arrest is a sudden and life-threatening emergency in which the heart abruptly stops pumping blood, leading to loss of consciousness and potential death within minutes. Conventional cardiopulmonary resuscitation (CPR) remains the first-line treatment, but even high-quality CPR restores only a fraction of normal cardiac output, often leaving vital organs, particularly the brain and heart, at risk of hypoxic injury. As a result, prolonged or refractory cardiac arrest frequently results in poor survival rates and significant neurological impairment.
Extracorporeal Cardiopulmonary Resuscitation (ECPR) has emerged as an advanced intervention for patients who do not respond to conventional CPR. By rapidly initiating extracorporeal membrane oxygenation (ECMO), ECPR temporarily takes over the heart and lung function, maintaining continuous blood flow and oxygen delivery to critical organs. This life-support technique not only prevents irreversible organ damage but also creates a vital window for clinicians to diagnose and treat reversible causes of cardiac arrest, such as acute myocardial infarction, pulmonary embolism, or severe electrolyte disturbances.
This blog explores the vital role of ECPR in cardiac arrest management, highlighting its key functions, benefits, and challenges.
What is ECPR?
Extracorporeal Cardiopulmonary Resuscitation (ECPR) is an advanced life-support technique used in patients experiencing cardiac arrest when conventional cardiopulmonary resuscitation (CPR) is unsuccessful. It involves the rapid initiation of extracorporeal membrane oxygenation (ECMO), which temporarily takes over the function of the heart and lungs by circulating oxygenated blood throughout the body.
By maintaining continuous blood flow and oxygen delivery to vital organs, particularly the brain and heart, ECPR helps prevent irreversible organ damage during prolonged resuscitation. This approach creates a critical window of time for healthcare providers to identify and treat reversible causes of cardiac arrest, such as acute coronary blockage or pulmonary embolism, improving the chances of survival and neurological recovery in carefully selected patients.
Why Is ECPR Needed in Cardiac Arrest Management?
Conventional cardiopulmonary resuscitation (CPR), even when performed optimally, generates only 20-30% of normal cardiac output. This limited circulation is often insufficient to meet the metabolic demands of vital organs during prolonged resuscitation efforts.
As a result, extended low-flow states can rapidly lead to:
- Severe hypoxic brain injury
- Multi-organ failure
- Poor neurological recovery
In cases of refractory cardiac arrest, where high-quality CPR and defibrillation fail to restore spontaneous circulation, Extracorporeal Cardiopulmonary Resuscitation (ECPR) plays a critical rescue role. By providing continuous circulatory and respiratory support, ECPR sustains organ perfusion and oxygenation, creating a vital window for definitive diagnosis and treatment of the underlying cause of cardiac arrest.
What are the Key Roles of ECPR in Cardiac Arrest Management?
ECPR supports cardiac arrest management by maintaining circulation and oxygenation, protecting the brain and vital organs, serving as a bridge to definitive treatments, aiding refractory cases, and enabling recovery or advanced cardiac therapies.
The key roles of ECPR in cardiac arrest management are explained as follows:
1. Providing Sustained Circulatory Support
The primary role of extracorporeal cardiopulmonary resuscitation (ECPR) is to maintain adequate circulation and oxygenation when the heart is unable to generate sufficient cardiac output. By delivering continuous extracorporeal blood flow, ECPR preserves cerebral perfusion, supports myocardial oxygen delivery, and prevents irreversible organ damage. This sustained circulatory support is particularly vital during prolonged or refractory resuscitation efforts, where conventional CPR alone cannot meet the metabolic demands of vital organs.
2. Protecting the Brain and Vital Organs
Neurological injury is a major determinant of poor outcomes following cardiac arrest, largely due to prolonged cerebral hypoxia. ECPR helps mitigate ischemic injury by ensuring consistent oxygen delivery to the brain and other vital organs while minimizing fluctuations in systemic blood flow. Additionally, the controlled hemodynamic environment created by ECPR enables optimized post-resuscitation care, contributing to higher rates of neurologically intact survival in appropriately selected patients.
3. Creating a Bridge to Definitive Treatment
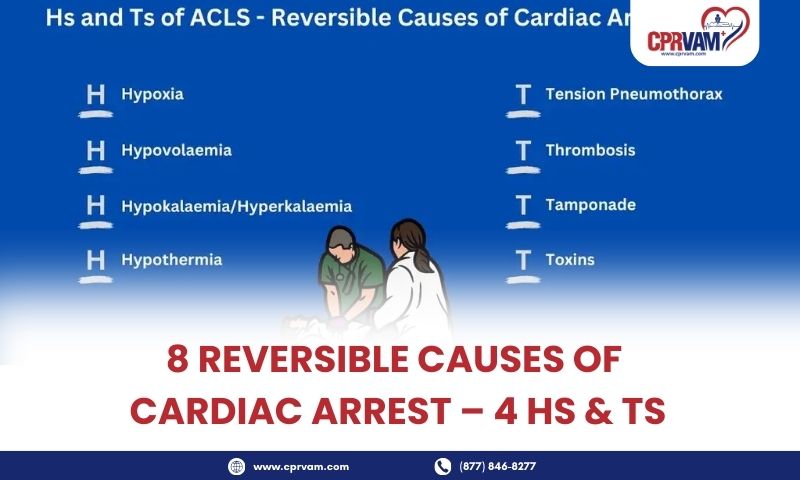
ECPR does not directly correct the underlying cause of cardiac arrest; rather, it provides critical time for diagnosis and definitive intervention. By maintaining stable circulation and oxygenation, ECPR allows clinicians to identify and treat reversible causes such as acute myocardial infarction, pulmonary embolism, drug toxicity, severe electrolyte imbalances, or hypothermia. During extracorporeal support, life-saving procedures such as coronary angiography, percutaneous coronary intervention, or thrombectomy can be performed safely and effectively.
4. Supporting Refractory Cardiac Arrest Cases
In modern cardiac arrest management, ECPR serves as an advanced rescue therapy for patients who fail to achieve return of spontaneous circulation despite high-quality CPR, defibrillation, and advanced cardiac life support interventions. In these refractory cases, ECPR provides a final opportunity to restore and maintain systemic perfusion, making it an essential component of advanced resuscitation pathways in specialized, ECMO-capable centers.
5. Acting as a Bridge to Recovery or Advanced Therapies
Beyond immediate resuscitation, ECPR can function as a bridge to myocardial recovery or more advanced therapeutic options. In selected patients, extracorporeal support allows time for cardiac function to recover or facilitates transition to long-term mechanical circulatory support devices or heart transplantation. This expanded role highlights the growing importance of ECPR not only as a resuscitation tool but also as a key element of comprehensive critical cardiac care.
What are The Benefits of ECPR in Cardiac Arrest Management?
ECPR improves survival and neurological outcomes in refractory cardiac arrest by ensuring continuous circulation and oxygenation. It protects vital organs, stabilizes patients for post-arrest care, and creates time for life-saving interventions and definitive treatment.
Here are the benefits of the ECPR in cardiac arrest management:
1. Improved Survival Rates
While the role of ECPR defines what it does, its benefits describe the outcomes achieved. One of the primary advantages is improved survival rates in selected patients. By providing continuous circulatory and oxygen support during cardiac arrest, ECPR significantly increases the likelihood of survival compared to conventional CPR alone.
2. Better Neurological Outcomes
ECPR helps maintain cerebral perfusion during prolonged resuscitation, reducing the risk of hypoxic brain injury. This results in better neurological outcomes, with a higher chance of survivors regaining functional independence and quality of life.
3. Reduced Hypoxic Organ Injury
Continuous oxygenation and circulation during ECPR protect vital organs from ischemic damage. By preventing prolonged low-flow states, ECPR minimizes hypoxic injury to the heart, kidneys, liver, and other critical organs.
4. Greater Ability to Manage Post-Cardiac Arrest Care
ECPR stabilizes patients, allowing clinicians to implement controlled and optimized post-resuscitation care. This includes targeted temperature management, hemodynamic optimization, and treatment of the underlying cause of cardiac arrest, which improves overall recovery outcomes.
5. Expanded Treatment Options for Other Fatal Cases
By maintaining circulation, ECPR provides time to perform life-saving interventions that might otherwise be impossible, such as coronary angiography, thrombectomy, or even preparation for heart transplantation. This expands treatment possibilities for cases that would otherwise have a very low chance of survival.
How Are Patients Selected for ECPR in Cardiac Arrest Management?
Patients are selected for ECPR based on witnessed arrest, short no-flow time, reversible causes, quality prior resuscitation, access to experienced teams, and patient factors such as age and comorbidities to maximize survival and neurological recovery.
Patients are selected for ECPR in cardiac arrest management based on the following criteria:
1. Witnessed Cardiac Arrest
ECPR is most effective in patients who experience a witnessed cardiac arrest, as early recognition allows rapid initiation of high-quality CPR and timely deployment of the extracorporeal circuit. Immediate intervention is critical to minimize low-flow or no-flow periods and improve survival outcomes.
2. Short No-Flow Time
Patients with minimal time without circulation (no-flow time) before resuscitation efforts begin are ideal candidates. Short no-flow intervals reduce the risk of irreversible organ and brain injury, making ECPR more likely to achieve favorable neurological outcomes.
3. Potentially Reversible Cause of Cardiac Arrest
ECPR is particularly indicated in cases where the cardiac arrest has a potentially reversible cause, such as acute myocardial infarction, pulmonary embolism, drug overdose, severe electrolyte disturbances, or hypothermia. Stabilizing circulation with ECPR provides a critical window for clinicians to treat these underlying conditions effectively.
4. Adequate Pre-Hospital or In-Hospital Resuscitation
Candidates should have received high-quality CPR and advanced life support prior to ECPR initiation. Proper resuscitation ensures that minimal perfusion is maintained while ECMO cannulation is performed, improving the likelihood of survival and recovery.
5. Access to Experienced ECPR Team and Resources
ECPR requires a specialized multidisciplinary team, rapid cannulation protocols, and advanced post-resuscitation care. Patients treated in centers with trained personnel, established protocols, and the necessary equipment are more likely to benefit from ECPR intervention.
6. Considering Age and Existing Health Conditions
While not absolute contraindications, younger patients with fewer comorbidities generally achieve better outcomes with ECPR. Patient selection should weigh the likelihood of meaningful recovery against the risks and resource intensity of the procedure.
What Are the Key Challenges and Limitations of ECPR?
ECPR faces challenges, including high costs, the need for specialized teams, limited availability, procedural risks, and strict time-sensitive patient selection. These limitations affect accessibility and outcomes, restricting its use to well-equipped centers and carefully chosen cardiac arrest patients.
Some of the challenges and limitations of ECPR are explained in foillowing:
1. High Resource and Cost Requirements
ECPR is a resource-intensive intervention that requires specialized equipment, trained personnel, and continuous monitoring. The costs associated with ECMO machines, disposables, and dedicated critical care teams can limit its availability to well-equipped centers.
2. Need for Skilled Multidisciplinary Teams
Successful ECPR implementation depends on a highly trained team, including emergency physicians, cardiologists, perfusionists, and critical care staff. Inexperienced or uncoordinated teams may delay cannulation, reduce effectiveness, or increase complication rates.
3. Limited Availability and Accessibility
ECPR is typically available only in specialized hospitals or centers with ECMO capability. Geographic limitations, transport delays, and lack of regional protocols can restrict timely access for patients who might benefit.
4. Risk of Complications
Like any invasive procedure, ECPR carries risks, including bleeding, vascular injury, infection, and thrombosis. Careful patient monitoring and adherence to protocols are essential to minimize these complications.
5. Time-Sensitive Patient Selection
ECPR is most effective when initiated early in carefully selected patients. Delays in recognition, prolonged low-flow periods, or inappropriate patient selection can significantly reduce survival and neurological outcomes, limiting the intervention’s overall effectiveness.
How Will ECPR Shape the Future of Cardiac Arrest Treatment?
ECPR is set to transform cardiac arrest treatment by improving access through specialized centers, advancing ECMO technology, refining patient selection, integrating with other resuscitation strategies, and expanding evidence-based training to enhance survival and outcomes.
Here’s how ECPR is expected to shape the future of cardiac arrest treatment:
1. Expanded Access and Regionalized Systems
As evidence supporting ECPR continues to grow, more hospitals and healthcare systems are developing ECMO-capable centers and regionalized cardiac arrest networks. Improved pre-hospital triage, rapid transport protocols, and coordination between emergency medical services and specialized centers are expected to increase timely access for eligible patients.
2. Advances in Technology
Ongoing improvements in ECMO technology, including smaller, more portable devices, automated flow control, and simplified cannulation techniques, are making ECPR faster, safer, and more widely deployable. These innovations may reduce procedure-related complications and expand use in out-of-hospital settings.
3. Refinement of Patient Selection and Protocols
Future research aims to refine clinical criteria for ECPR, identifying patients most likely to benefit. Optimizing timing, minimizing low-flow intervals, and integrating predictive models will help improve survival rates and neurological outcomes while reducing unnecessary interventions.
4. Integration with Advanced Resuscitation Strategies
ECPR is expected to become increasingly integrated with other advanced cardiac arrest interventions, including targeted temperature management, early coronary intervention, and mechanical circulatory support. Coordinated, protocol-driven care will enhance overall outcomes for patients with refractory cardiac arrest.
5. Evidence-Based Guidelines and Training
As clinical data accumulates, standardized guidelines and training programs for ECPR are likely to expand globally. Emphasis on education, simulation, and protocol adherence will improve team readiness, procedural efficiency, and patient outcomes, making ECPR a mainstay of advanced cardiac arrest care.
Get Ready to Save Lives with Advanced CPR Training
Extracorporeal Cardiopulmonary Resuscitation (ECPR) is a life-saving intervention in cardiac arrest management that provides continuous circulatory and oxygen support when conventional CPR fails. It improves survival rates, protects the brain and vital organs, and serves as a bridge to definitive treatment or advanced therapies. Optimal outcomes depend on early initiation, careful patient selection, and trained multidisciplinary teams. With technological advancements and standardized protocols, ECPR is becoming a cornerstone of advanced resuscitation care, offering critically ill patients a higher chance of recovery and neurologically intact survival.
To effectively contribute in such critical situations, healthcare providers and first responders need specialized training that builds both skills and confidence. CPR VAM can help with this, offering American Heart Association (AHA) certified courses in CPR, BLS, ACLS, and PALS, designed to equip you with the knowledge and hands-on experience to respond confidently in cardiac emergencies, including advanced interventions like ECPR.