When the heart suddenly stops, every second matters. Two critical rhythms, Pulseless Ventricular Tachycardia (pVT) and Ventricular Fibrillation (VF), are leading causes of cardiac arrest in the United States. Both are considered shockable rhythms, meaning they often respond to defibrillation and CPR. In out-of-hospital cardiac arrests, these rhythms are present in approximately 23-30 % of cases, and rapid intervention significantly increases survival.
Pulseless VT and VF appear differently on an electrocardiogram, but both prevent the heart from pumping effectively. VF causes the ventricles to quiver due to disorganized electrical activity, while pVT produces a very fast but organized rhythm without a pulse. Despite these differences, treatment in emergencies is the same with immediate CPR and defibrillation. Quick recognition and action can be life-saving.
This blog breaks down the key differences between Pulseless Ventricular Tachycardia and Ventricular Fibrillation, including ECG signs, causes, treatments, and emergency care steps to help save lives during cardiac arrest.
Why Are Ventricular Arrhythmias Important in Clinical Practice?
Ventricular arrhythmias are abnormal heart rhythms that start in the heart’s lower chambers, the ventricles. They can cause the heart to pump ineffectively or stop altogether. These rhythms are dangerous because they can quickly lead to sudden cardiac arrest. Recognizing and treating them immediately is critical to saving lives and improving patient outcomes.
Ventricular arrhythmias disrupt the heart’s ability to circulate blood effectively. When the ventricles beat too fast or irregularly, the heart cannot pump properly. This can stop blood flow to vital organs, making these conditions life-threatening.
Key Points
Ventricular arrhythmias are a leading cause of sudden cardiac arrest.
VF and pVT account for a large proportion of out-of-hospital and in-hospital cardiac arrests.
Immediate rhythm recognition directly impacts survival.
How Does Ventricular Fibrillation Affect Heart Function?
Ventricular fibrillation, or VF, is a life-threatening heart rhythm problem in which the lower chambers of the heart, called the ventricles, quiver instead of contracting properly. This prevents blood from moving through the body, resulting in no pulse and no circulation. Immediate recognition and treatment are critical to survival, as every second counts.
Ventricular fibrillation is defined by chaotic, disorganized ventricular electrical activity with no effective mechanical contraction. The ventricles quiver rather than contract, producing no forward blood flow and no pulse.
Key Characteristics of VF
The heart shows completely irregular electrical activity.
There are no identifiable P waves or QRS complexes on the ECG.
The ventricular rate cannot be measured.
This rhythm causes immediate circulatory collapse.
Common Associated Causes
Acute myocardial ischemia or infarction can trigger this condition.
Hypoxia may lead to the development of this rhythm.
Electrolyte abnormalities can disrupt normal cardiac electrical activity.
Severe trauma can precipitate this condition.
Exposure to certain drugs or toxins can cause this rhythm disturbance.
Electrocardiographic Signs
- It shows a rapid, irregular, and chaotic cardiac rhythm in which there are no clearly identifiable QRS complexes or P waves on the ECG, indicating disorganized electrical activity in the heart.
How Does Pulseless Ventricular Tachycardia Impact Circulation?
Pulseless ventricular tachycardia, or pVT, is a life-threatening heart rhythm where the ventricles beat very rapidly, usually between 150 and 250 beats per minute, but fail to pump blood effectively. Electrical activity is present, yet the heart cannot fill or eject blood properly, leaving no pulse and no circulation. Immediate recognition and intervention are critical to improve survival.
If you see a fast, organized heartbeat without a palpable pulse, it could be pVT. This condition often occurs in people with heart disease and can quickly deteriorate into ventricular fibrillation if left untreated. Timely action can save lives.
Defining Features of pVT
The rhythm is regular and fast, with wide QRS complexes visible on the ECG.
The ventricular rate is measurable.
There is organized electrical activity present despite the absence of a palpable pulse.
This rhythm is often associated with ischemic or structural heart disease.
Clinical Notes
Pulseless ventricular tachycardia may develop from ventricular tachycardia that initially has a palpable pulse.
If left untreated, pulseless ventricular tachycardia can worsen and deteriorate into ventricular fibrillation.
Electrocardiogram (ECG) Features
- Displays a rapid, regular rhythm with wide QRS complexes above 150 beats per minute, yet fails to generate effective blood flow.
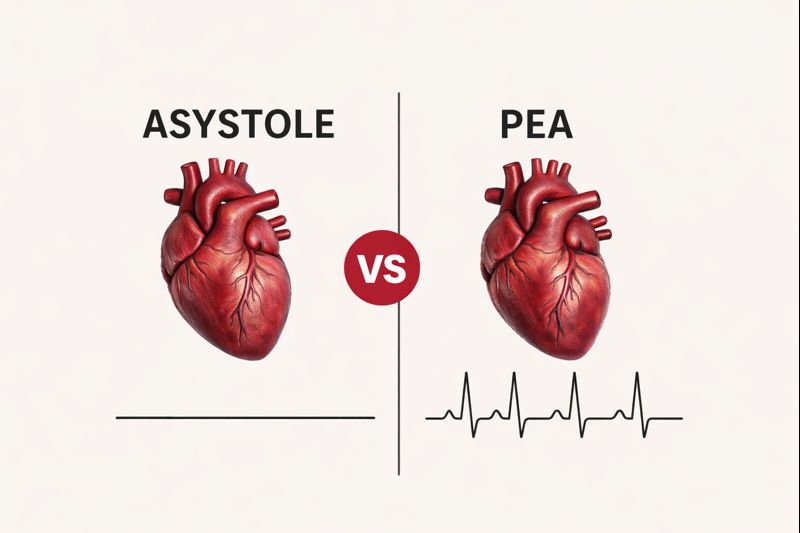
How Can Ventricular Fibrillation and Pulseless VT Be Differentiated?
Ventricular fibrillation (VF) and pulseless ventricular tachycardia (pVT) are both life-threatening heart rhythms that require immediate attention. You should know that while the emergency treatment for VF and pVT is the same, their ECG patterns, electrical activity, and heart behavior are different. Understanding these differences can help you recognize the rhythm and anticipate the risks.
You may notice that VF shows chaotic, disorganized electrical activity with no effective contraction, while pVT appears regular and organized but still fails to pump blood effectively. Being able to distinguish between the two can help you stay informed and improve awareness in emergencies.
Key Differences Between Ventricular Fibrillation (VF) and Pulseless Ventricular Tachycardia (pVT)
Features | Ventricular Fibrillation (VF) | Pulseless Ventricular Tachycardia (pVT) |
ECG Rhythm | Chaotic and disorganized | Regular and organized |
QRS Complexes | Absent or unrecognizable | Wide and identifiable |
Heart Rate | Unmeasurable | Typically 150-250 bpm |
Pulse | Absent | Absent |
Electrical Pattern | No consistent waveform | Monomorphic or polymorphic |
Mechanical Activity | No effective contraction | Ineffective contraction |
Clinical Impact | Immediate circulatory collapse | Circulatory collapse, sometimes with a slightly better prognosis |
Common Causes | Ischemia, trauma, electrolyte disturbances, and drug toxicity | Ischemia, previous heart disease, and electrolyte disturbances |
Response to Drugs | Epinephrine and Amiodarone after shock | Epinephrine and Amiodarone after shock |
Clinical Insight: VF and pVT require identical management during cardiac arrest, even though their ECG appearances differ.
How Are VF and Pulseless VT Managed During Cardiac Arrest?
Ventricular fibrillation (VF) and pulseless ventricular tachycardia (pVT) are life-threatening rhythms that require immediate action. You should know that following the BLS algorithms and ACLS cardiac arrest algorithms is essential for survival. Rapid recognition, high-quality CPR, and timely defibrillation are the cornerstones of management, and being prepared can make a critical difference in patient outcomes.
The following steps outline how to manage VF and pulseless VT during cardiac arrest:
1. High-Quality CPR
You should perform CPR with chest compressions immediately. Maintain the correct depth and rate, and minimize interruptions. This ensures adequate blood flow to the brain and heart, improving the chances of survival.
CPR Essentials
Initiate chest compressions immediately
Maintain adequate depth and rate
Minimize interruptions to support coronary and cerebral perfusion
2. Defibrillation
VF and pVT are both shockable rhythms, so early defibrillation is crucial. You should deliver unsynchronized shocks as soon as possible, as rapid defibrillation greatly increases survival chances.
Defibrillation Priorities
VF and pVT are shockable rhythms
Deliver unsynchronized defibrillation promptly
Early defibrillation significantly improves survival
3. Advanced Cardiac Life Support
You should resume CPR immediately after each shock. Establish IV or IO access, give medications as indicated, and continuously monitor the rhythm and patient response. Following ACLS protocols maximizes effectiveness.
ACLS Critical Steps
Resume CPR immediately after each shock
Establish IV or IO access
Administer medications as indicated
Continuously reassess rhythm and patient response
Which Medications Are Used for VF and Pulseless VT?
When defibrillation and CPR alone do not restore circulation, medications can support resuscitation efforts. You should know that these drugs help improve heart rhythm, support blood flow to vital organs, and increase the chance of survival during cardiac arrest.
The following medications are used for managing VF and pulseless VT:
Epinephrine
Purpose: Improves coronary and cerebral perfusion
Dose: 1 mg IV/IO every 3-5 minutesAmiodarone
Purpose: Antiarrhythmic for refractory VF or pVT
Dose: 300 mg IV/IO initial dose, 150 mg IV/IO repeat doseLidocaine (Alternative)
Purpose: Alternative antiarrhythmic
Dose: 1-1.5 mg/kg IV/IO initial, 0.5-0.75 mg/kg additional dosesMagnesium Sulfate
Purpose: Indicated for torsades de pointes
Dose: 2 g IV/IO
Why Is Treating Reversible Causes Critical After ROSC?
After return of spontaneous circulation (ROSC), identifying and treating reversible causes is essential. You should know that correcting these factors helps prevent another cardiac arrest and improves brain function. Failing to address them can quickly lead to recurrence and worsen overall patient outcomes.
You should carefully evaluate the common reversible causes in ACLS (Hs and Ts), which include hypovolemia, hypoxia, acidosis, electrolyte imbalances, hypothermia, and other factors. By systematically addressing these issues, you can help stabilize the patient and support full recovery after ROSC, which is a core principle of post–cardiac arrest care.
Common Reversible Causes (Hs and Ts)
Hypovolemia
Hypoxia
Hydrogen ion (Acidosis)
Hypo-/hyperkalemia
Hypothermia
Tension pneumothorax
Cardiac tamponade
Toxins
Thrombosis (coronary or pulmonary)
Trauma
Essential Takeaways for VF and Pulseless VT Management
Ventricular fibrillation and pulseless ventricular tachycardia are life-threatening rhythms where every second counts. You should act immediately with high-quality CPR and early defibrillation, supported by medications when needed. Recognizing ECG patterns, understanding underlying causes, and addressing reversible factors after ROSC are critical for survival. Quick, informed action can save lives, stabilize patients, and improve outcomes.
Emergencies won’t wait, and neither should you. At CPR VAM, an AHA-approved training center, you’ll gain the skills and confidence to respond effectively to VF and pulseless VT. Our BLS and ACLS certification courses offer hands-on training and proven life-saving techniques. Sign up now and be ready to act decisively, protect lives, and make a real difference when every second matters.